Original Article: JRCRS. 2025; 13(4):215-220
5- Role of Self-Managed, Semi-Supervised Physical Therapy in Urinary Incontinence Rehabilitation: A Quasi Pre-Post Experimental Trial
Anashia Aftab1, Seema Gul2
1 Physical therapist, Hamad medical corporation, Qatar
2 Lecturer, Khyber Medical University, Peshawar, Pakistan
Full-Text PDF DOI: https://dx.doi.org/10.53389/JRCRS.2025130405
ABSTRACT:
Background: Urinary incontinence (UI) is widely recognized as a debilitating condition. Regardless of its type, UI can significantly affect an individual’s quality of life across multiple domains, including emotional well-being, functional capacity, and social participation. A comprehensive physical rehabilitation program has been shown to offer beneficial effects in the management of urinary incontinence.
Objective: To determine the role of self-managed, semi-supervised physical therapy in urinary incontinence rehabilitation.
Methodology: This was a quasi-experimental clinical trial, conducted at Lady Reading Hospital, Peshawar, involving patients diagnosed with urinary incontinence. Based on predefined inclusion criteria, a total of 31 participants were recruited through a convenience sampling technique. The sample comprised 9 male and 22 female patients, with a mean age of 40.93 ± 13.9 years. All participants underwent a comprehensive, self-managed, semi-supervised rehabilitation program over a period of four weeks. Bladder behavior—including the severity, frequency, and volume of urine leakage—was recorded. The effectiveness of the intervention was evaluated using the International Consultation on Incontinence Questionnaire–Short Form (ICIQ-SF).
Results: The results of this study show that 45.16 % participants were suffering from Stress Urinary Incontinence (SUI); 25.80% complained of Urge Urinary Incontinence (UUI) and 29.03% were having symptoms of both SUI and UUI so they were classified as Mixed Urinary Incontinence (MUI). The paired t-test for the comparison of bladder-related quality of life at baseline (ICIQF initial =12.37 + 3.64) and at the end of the treatment (ICIQF final =5.44 + 3.61) shows clinically and statistically significant results. (p=0.01).
Conclusion: This study determines that a self-managed and semi-supervised physical rehabilitation protocol can be effectively implemented in patients with any type of urinary incontinence to improve bladder related quality of life.
Keywords: Physical Therapy, Urinary Incontinence, Quality of Life
Introduction:
The International Continence Society defines urinary incontinence (UI) as the unintentional and involuntary loss of urine.1 When urine leakage occurs during physical exertion, such as sneezing or coughing, it is classified as Stress Urinary Incontinence (SUI).2 In contrast, Urge Urinary Incontinence (UUI) refers to the involuntary loss of urine associated with a sudden, intense urge to urinate.3 The causes of SUI include weak pelvic floor muscles, poor sphincter control, and bladder hypermobility.4 In comparison, UUI typically results from detrusor over activity, bladder irritation, or loss of neurogenic control, which may occur in conditions such as stroke, multiple sclerosis, or Parkinson’s disease.5 Sometimes patients present with a combination of both SUI and UUI. This type of incontinence is usually classified as Mixed Urinary Incontinence (MUI).
UI is a global medical condition that is often underestimated. Literature highlights a significant burden of UI, particularly in developing countries where many cases remain undiagnosed.6 The overall prevalence of UI in South Asia is reported to be 14.2% (95% CI: 6.1–29.8).7 Women are at a significantly higher risk (around 13.9%) of developing urinary incontinence than men (2.7%).8 Stress urinary incontinence is the most prevalent subtype among women, with reports showing rates as high as 59.4% in healthy female populations. 9 Urge incontinence follows with a prevalence of 31.1% in women.10 Furthermore, mixed urinary incontinence (MUI) is reported by about 20% of men and 33% of women.11, 12 In USA, the prevalence of urinary incontinence was 15.7 % in women & 5.3 % in men.13, 14 The overall prevalence of UI in Pakistan was estimated as 11% with 4.7 %SUI, 3.2% UUI and 2.85%Mixed UI.15 A study reported that UI was the most common pelvic floor disorder reported, with a prevalence of 17.1%.16 Moreover UI symptoms are more significant with increasing age i-e; 12.2% for <60 years &23.8% for >60 years.17
UI poses a high economic burden, estimated at $3.3 million.18 In the European Union, the average annual per-patient cost of UI is approximately EUR€1,700.0, with women bearing nearly four times the financial burden compared to men.19 The diagnosis of urinary incontinence (UI) involves a comprehensive process aimed at identifying the underlying causes. The initial step includes evaluating potential differential diagnoses such as delirium, atrophic vaginitis, hyperglycemia, pharmaceutical side effects, functional incontinence, urinary tract infections (UTIs), and stool impaction. These conditions must be ruled out before proceeding. Once excluded, various validated subjective assessments and investigations are utilized to determine the specific type of chronic urinary incontinence, such as stress, urge, or mixed incontinence.20
The American College of Physicians recommends conservative treatment as the primary and most effective approach for managing urinary incontinence (UI). This approach includes identifying red flags, classifying the type of UI, implementing behavioral modifications, engaging in pelvic floor muscle training, and, when appropriate, using medications. The recommended duration for this conservative regimen is typically 6 to 8 weeks. If no significant improvement is observed during this period, patients may then be referred for surgical intervention.21
According to a recent study, urinary incontinence (UI) is prevalent among women in Pakistan, with a reported rate of 32%. Among those affected, the distribution of stress urinary incontinence (SUI), urge urinary incontinence (UUI), and mixed urinary incontinence (MUI) was 35.71%, 40.11%, and 24.73%, respectively. The quality of life in these individuals was significantly impacted, with 69.3% reporting a negative effect due to UI. Despite this, very few sought medical attention through outpatient departments (OPDs) or clinics.22
Based on literature, Urinary incontinence is a common yet underreported condition that significantly impacts quality of life, especially among women in developing countries like Pakistan.
Conventional management strategies, such as pelvic floor muscle training and bladder retraining, are typically delivered through frequent face-to-face sessions with healthcare providers. However, these approaches may not be feasible for all patients due to barriers such as time constraints, travel limitations, cost, and limited access to specialized care. As a result, adherence to therapy is often poor, leading to suboptimal outcomes.23 Traditional clinical management approaches often require frequent visits to healthcare providers, which may not be feasible for all patients. There is a dire need for accessible, cost-effective, and sustainable interventions that empower individuals to manage their condition independently. Therefore, this study aims at finding the effectiveness of a rehabilitation program for treating urinary incontinence semi-supervised by professional physical therapist and educating patients remotely about bladder management strategies without frequent visits to hospital.
Methodology
This quasi-experimental study was conducted after obtaining ethical approval from the review boards of Khyber Medical University (DIR/KMU-AS&RB/OS/000960) and Lady Reading Hospital, Peshawar (Ethical Code: Reference No.196/LRH). Participants were recruited using a convenience sampling technique. The required sample size was calculated as 31 using the Openepi sample size calculator with 95% confidence interval and 5% margin error. In accordance with criteria used in previous studies, individuals aged 18 years and above—both male and female—were eligible for inclusion if they had been clinically diagnosed with urinary incontinence (UI) by a urologist or gynecologist. Exclusion criteria included the presence of any of the following conditions: (1) neurogenic bladder, (2) malignancy, (3) impaired ambulation, (4) impaired cognition (5) drugs induced incontinence, (6) Hyperglycemia or (7) UTIs. Once eligibility was confirmed, each participant was provided with an information sheet, and written informed consent was obtained prior to enrollment in the study.
Demographic details were collected from all study participants. Baseline bladder-related quality of life and intensity of UI was assessed using the Urdu version of the short form of the International Consultation on Incontinence Questionnaire (ICIQ-SF).It is a reliable tool for assessing urinary incontinence in the Pakistani population.24 Following are the psychometric details of Urdu version of ICIQ-SF (internal consistency Cronbach’s alpha coefficient =0.791, Content validity = 0.93 -0.97. Test-retest reliability -Intraclass correlation coefficient (ICC) = 0.903).25
Following this assessment, patients received a structured rehabilitation protocol as part of their urinary incontinence (UI) management. The intervention included the following components: (1) Kegel exercises, (2) the Knack technique, (3) bladder training. All patients received comprehensive training during the initial contact session at hospital. Pamphlets containing the exercise regimen and detailed instructions were provided as handouts as home plan. The program was implemented over a period of six weeks. To ensure adherence and provide supervision, participants were contacted once weekly via telephone for 6 weeks.
Kegel exercises: participants were trained by a physical therapist to activate and relax the pelvic floor muscles (PFM) in various static and dynamic positions, including supine, bridging, cat-camel, long sitting, cross sitting, and standing with heel raises. Each session consisted of 10 repetitions followed by a 5-second rest, then another 10 repetitions, completing a total of two sets. participants were advised to perform these exercises three times per day.26
Knack technique: participants were also trained to consciously contract the pelvic floor muscles (PFM) before engaging in activities that increase intra-abdominal pressure, such as sneezing, coughing, or lifting.27
Bladder Training: A bladder diary was provided to all participants to monitor their voiding patterns. They were educated on how to incorporate a fixed voiding schedule into their daily routine and guided on gradually increasing the time intervals between toilet visits to improve bladder control.28
All study participants completed 6-weeks rehabilitation protocol and were re-assessed at the end of the study.
Data was analyzed using SPSS (Statistical Package for Social sciences) version 23. Mean and standard deviations were obtained to determine sample characteristics. For comparison between variable before and after the implantation of rehabilitation protocol, paired t-test was used. Intervention was considered effective at P ≤ 0.05. To ensure the validity of the test, assumptions of normality for the difference scores were assessed. The distribution of pre–post difference scores was examined using the Shapiro–Wilk test (P ≥ 0.001).
Results
A total of 31 participants were included in the study, with a mean age of 40.93 ± 13.90 years. Both male and female participants were enrolled. The study population included patients from various regions of Khyber Pakhtunkhwa. (Table 1)
| Table 1: Demographic Details of the Sample | |
| Variables | Frequency |
| No of participants | n=31 |
| Age (Mean ± SD) | 40.93 ± 13.90 years |
| Gender | Male: 9(29.03%) |
| Female: 22(70.96%) | |
| Location | Local 20(66.66%)
Distant 11(35.48%) |
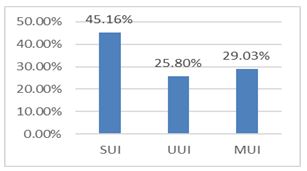
The distribution of UI was depicted using frequency tables showing that 45.16 % participants were suffering from SUI; 25.80% complained of UUI and 29.03% were having symptoms of both SUI and UUI so they were classified as MUI. (Figure 1)
Figure 1: Distribution of Urinary Incontinence across Participants
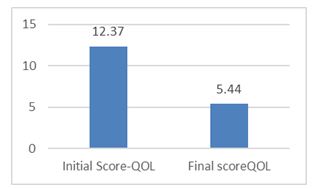
The bladder-related quality of life of participants was assessed using ICIQ-SF. To evaluate the effectiveness of the rehabilitation protocol, a paired t-test was applied to compare the scores obtained at baseline with those recorded at the end of the six-week intervention. The post-test scores (5.44 ± 3.61) were significantly lower than pre-test scores (12.37 ± 3.47). The mean decrease indicated a large effect size, d = 1.98, Hedges’ g = 1.93. (see table2, figure 2)
To ensure the validity of the test, assumptions of normality for the difference scores were assessed. The distribution of pre–post difference scores was examined using the Shapiro–Wilk test. The results indicated that the normality assumption was reasonably met and no outliers were detected.
| Table 2: Change in Patient Reported Bladder-Related Quality of Life-Score | ||||
| Mean | SD | p-value | Effect size | |
| Pre-ICIQF | 12.37 | 3.47 | 0.001 | > 0.8 (large) |
| Post- ICIQF | 5.44 | 3.61 | ||
Figure 2: change in patient reported bladder-related quality of life-score
Discussion
This study demonstrated that self-managed, semi-supervised Kegel exercises combined with bladder training and knack technique is an effective approach in improving all types of urinary incontinence. The supervision can be maintained by a telephonic interaction so minimizing the number of visits to the OPD or clinics.
In this study, we observed that prevalence of UI is high in both men and women but the ratio is comparatively higher in women (70.96%) than in men (22.58%). These findings are in accordance to the findings of the Fourth International Consultation on Incontinence 2010. The gathered information suggest that UI is more common in women worldwide varying 25 to 45%. The men are affected by half of the women population (11 to 34%).29
A study shows that prevalence of stress and mix urinary incontinence is higher than urge incontinence.30 Contrary the pattern of distribution of UI in our study, suggested that SUI is the most common type of UI (45.16%). MUI (29.03%) is the second common type followed by UUI (25.89%). This difference can be justified by the work of Haylon et al. He concluded in his study that the data regarding the true prevalence of different types of urinary incontinence vary across different studies depending on type of population, social stigma and behavior of people for seeking clinical attention for UI.31
A study was conducted which targets a specific population of elderly women (n= 49) with UI. This study used a community-based education approach. All the participants were educated about bladder function, pelvic floor exercises and life style modification. At the end of the treatment, the participants reported decrease frequency of UI and improved urinary control.32 A similar study was conducted on elderly women by — et al. A total n=164 participants were educated in 2-hour lecture about behavioral modification and pelvic floor muscle training. The outcomes were then compared with a control group n=195 after 1 year. The treatment group was statistically significant p=0.0001 in terms of voiding interval and PFM strength.33 These findings are in accordance with our study as incorporation of physical therapy and bladder training both showed a significant decrease in ICIQF scoring that demonstrates an improved UI intensity and QOL associated with UI.
An extensive systematic review suggests that PFM and bladder training can resolved incontinence (pooled risk difference, 0.13 [95% CI, 0.07 to 0.20). According to the author, these findings are questionable as treatment techniques vary highly across the trials. The variation is also observed in the assessment of UI, selection criteria for the study, sampling technique and tools used to determine the effectiveness of different protocols.34
Limitation: This is a single group quasi-experimental study with very small sample size and no control group. Therefore, the true generalizability of its findings is limited.
Recommendation: This study gives an insight into clinical implication and effectiveness of urinary incontinence rehabilitation when given semi-supervised and self-managed by patients. However, in future, a comparable control group along true randomization and a larger sample size can be added in this clinical trial to get a high-level evidence regarding the effectiveness of semi-supervised, self-managed rehabilitation protocol.
Conclusion
This study determines that a self-managed and semi-supervised physical rehabilitation protocol can be effectively implemented in patients with any type of urinary incontinence to improve bladder related quality of life.
References
- Doumouchtsis SK, de Tayrac R, Lee J, Daly O, Melendez-Munoz J, Lindo FM, et al. An International Continence Society (ICS)/International Urogynecological Association (IUGA) joint report on the terminology for the assessment and management of obstetric pelvic floor disorders. International urogynecology journal. 2023;34(1):1-42.
- Al-Ahmadi FQ, Awaji NAM, Alshehri HA, Almotairi SA, Alharbi AMF, Asiri AAM, et al. Urinary Incontinence Diagnosis and Management and its Impact in Woman’s Health Quality of Life. Journal of International Crisis and Risk Communication Research. 2024;7(S6):1401.
- Leslie SW, Tran LN, Puckett Y. Urinary incontinence. 2024.
- Bergström BS. Stress urinary incontinence is caused predominantly by urethral support failure. International Urogynecology Journal. 2022;33(3):523-30.
- Alves JO, Da Luz ST, Brandão S, Da Luz CM, Jorge RN, Da Roza T. Urinary incontinence in physically active young women: prevalence and related factors. International journal of sports medicine. 2017;38(12):937-41.
- Lukacz ES, Santiago-Lastra Y, Albo ME, Brubaker L. Urinary incontinence in women: a review. Jama. 2017;318(16):1592-604.
- Mostafaei H, Sadeghi‐Bazargani H, Hajebrahimi S, Salehi‐Pourmehr H, Ghojazadeh M, Onur R, et al. Prevalence of female urinary incontinence in the developing world: A systematic review and meta‐analysis—A Report from the Developing World Committee of the International Continence Society and Iranian Research Center for Evidence Based Medicine. Neurourology and urodynamics. 2020;39(4):1063-86.
- Bedretdinova D, Fritel X, Zins M, Ringa V. The effect of urinary incontinence on health-related quality of life: is it similar in men and women? Urology. 2016; 91:83-9.
- Rubilotta E, Balzarro M, D’Amico A, Cerruto MA, Bassi S, Bovo C, et al. Pure stress urinary incontinence: analysis of prevalence, estimation of costs, and financial impact. BMC urology. 2019;19(1):44.
- Abufaraj M, Xu T, Cao C, Siyam A, Isleem U, Massad A, et al. Prevalence and trends in urinary incontinence among women in the United States, 2005–2018. American journal of obstetrics and gynecology. 2021;225(2):166. e1-. e12.
- Bortolotti A, Bernardini B, Colli E, Di Benedetto P, Giocoli Nacci G, Landoni M, et al. Prevalence and risk factors for urinary incontinence in Italy. European urology. 2000;37(1):30-5.
- Sultana A, Najeeya A, Rahman K, Saeedi R, Khanam M. Mixed Urinary Incontinence (MUI) in Women: From Evidence to Clinical Practice. Journal of Health Science Research. 2020;5(2):39-50.
- Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, et al. Prevalence of symptomatic pelvic floor disorders in US women. Jama. 2008;300(11):1311-6.
- Tennstedt SL, Link CL, Steers WD, McKinlay JB. Prevalence of and risk factors for urine leakage in a racially and ethnically diverse population of adults: the Boston Area Community Health (BACH) Survey. American journal of epidemiology. 2008;167(4):390-9.
- Jokhio A, Rizvi R, Rizvi J, Macarthur C. Urinary incontinence in women in rural Pakistan: prevalence, severity, associated factors and impact on life. BJOG: An International Journal of Obstetrics & Gynaecology. 2013;120(2):180-6.
- Wu JM, Vaughan CP, Goode PS, Redden DT, Burgio KL, Richter HE, et al. Prevalence and trends of symptomatic pelvic floor disorders in US women. Obstetrics and gynecology. 2014;123(1):141.
- Herschorn S, Gajewski J, Schulz J, Corcos J. A population‐based study of urinary symptoms and incontinence: the Canadian Urinary Bladder Survey. BJU international. 2008;101(1):52-8.
- Bettez M, Le Mai Tu KC, Corcos J, Gajewski J, Jolivet M, Bailly G. 2012 update: guidelines for adult urinary incontinence collaborative consensus document for the Canadian Urological Association. Canadian Urological Association Journal. 2012;6(5):354.
- Bishop C, Rodriguez-Cairoli F, Hagens A, Bermudez MA, Van Kerrebroeck P, Collen S. Prevalence, Socioeconomic, and Environmental Costs of Urinary Incontinence in the European Union. European Urology. 2025.
- Khandelwal C, Kistler C. Diagnosis of urinary incontinence. American Family Physician. 2013;87(8):543-50.
- DeMaagd GA, Davenport TC. Management of urinary incontinence. Pharmacy and Therapeutics. 2012;37(6):345.
- Fahim F, Fahim WB, Lakhta G, Khan FR. Urinary Incontinence in Pakistani Women: Impact on Quality of Life and Treatment-Seeking Behavior. Prog Med Sci. 2022;6(1):1-7.
- Sayner AM, Tang CY, Toohey K, Mendoza C, Nahon I. Opportunities and capabilities to perform pelvic floor muscle training are critical for participation: a systematic review and qualitative meta-synthesis. Physical therapy. 2022;102(10): pzac106.
- SF I-U. International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form (ICIQ-UI SF) [cited 2025 October 4, 2025]. Available from: https://iciq.net/iciq-ui-sf.
- Amon ZH, Ikram M, Ishtiaq I, Hayat R, Hussain SA. Urdu Translation and Cross-Cultural Validation of International Consultation on Incontinence Questionnaire Over Active Bladder (ICIQ-OAB). NeuroQuantology. 2023;21(6):1482-9.
- Park S-H, Kang C-B, Jang SY, Kim BY. Effect of Kegel exercise to prevent urinary and fecal incontinence in antenatal and postnatal women: systematic review. Journal of Korean Academy of Nursing. 2013;43(3):420-30.
- Fitz FF, Gimenez MM, de Azevedo Ferreira L, Matias MMP, Bortolini MAT, Castro RA. Effects of voluntary pre-contraction of the pelvic floor muscles (the Knack) on female stress urinary incontinence—a study protocol for a RCT. Trials. 2021; 22:1-12.
- Roloff KL. Effect of Provider Education on Urinary Incontinence Knowledge and Assessment. 2020.
- Buckley BS, Lapitan MCM. Prevalence of urinary incontinence in men, women, and children—current evidence: findings of the Fourth International Consultation on Incontinence. Urology. 2010;76(2):265-70.
- Nitti VW. The prevalence of urinary incontinence. Reviews in urology. 2001;3(Suppl 1): S2.
- Haylen BT, De Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourology and Urodynamics: Official Journal of the International Continence Society. 2010;29(1):4-20.
- Mcfall SL, Yerkes AM, Cowan LD. Outcomes of a small group educational intervention for urinary incontinence: episodes of incontinence and other urinary symptoms. Journal of Aging and Health. 2000;12(2):250-67.
- Diokno AC, Sampselle CM, Herzog AR, Raghunathan T, Hines S, Messer KL, et al. Prevention of urinary incontinence by behavioral modification program: a randomized, controlled trial among older women in the community. The Journal of urology. 2004;171(3):1165-71.
- Shamliyan TA, Kane RL, Wyman J, Wilt TJ. Systematic review: randomized, controlled trials of nonsurgical treatments for urinary incontinence in women. Annals of internal medicine. 2008;148(6):459-73.
|
Copyright Policy All Articles are made available under a Creative Commons “Attribution-NonCommercial 4.0 International” license. (https://creativecommons.org/licenses/by-nc/4.0/). Copyrights on any open access article published by Journal Riphah college of Rehabilitation Science (JRCRS) are retained by the author(s). Authors retain the rights of free downloading/unlimited e-print of full text and sharing/disseminating the article without any restriction, by any means; provided the article is correctly cited. JRCRS does not allow commercial use of the articles published. All articles published represent the view of the authors and do not reflect the official policy of JRCRS. |