Original Article: JRCRS.2025:13(3):165-171
8- Anxiety and Depression among Primary Caregivers of Male versus Female Children with Cerebral Palsy: A Cross-Sectional Comparative Study in Karachi, Pakistan
Ammara Rafique1
1 Lecturer, Indus College of Physical Therapy & Rehabilitation, Indus University of Health Sciences, Karachi, Pakistan
Full-Text PDF DOI: https://dx.doi.org/10.53389/JRCRS.2025130308
Abstract:
Background: Cerebral palsy (CP) is a neurological disorder that impacts movement, posture, and muscle tone due to brain damage in fetal development, infancy, or early childhood.
Objective: To compare anxiety and depression among primary caregivers of male versus female children with cerebral palsy.
Methodology: This cross-sectional comparative study was carried out between February 2020 and March 2021 with the caregivers of CP-inflicted children admitted at a rehabilitation center in Karachi, Pakistan. Among 46 approached caregivers, only 30 (75%) voluntarily participated in the study. Group 1 encompassed caregivers of male CP-inflicted patients (n=19) and group 2 encompassed caregivers of female CP-inflicted patients (n=11). Data on physical characteristics and additional impairments accompanying CP was gathered whereas face-to-face meetings were arranged with primary caregivers to gather data for sociodemographic questionnaire and Hospital anxiety depression scale (HADS).
Results: No significant differences were observed in the two groups concerning the physical characteristics of CP cases and sociodemographic characteristics of caregivers. Compared to the caregivers of female CP children, caregivers of male CP children had significantly higher anxiety (7.09±1.64; 8.42±1.6, p=0.044), depression (5.90±1.8; 8.10±1.88, p=0.004) and total HADS scores (6.50±1.79; 8.26±1.75, p=0.006).
Conclusion: Caregivers of male CP children were more prone to anxiety and depression problems. There was no significant correlation found between the sociodemographic profile of the caregivers and the characteristics of CP with the gender of CP children.
Keywords: Anxiety; Caregivers; Cerebral Palsy; Children; Depression; Pakistan
Introduction:
Cerebral palsy (CP) is a neurological disorder that impacts movement, posture, and muscle tone due to brain damage in fetal development, infancy, or early childhood.1 The worldwide incidence of CP is estimated at around 1.6 per 1,000 live births.2 However, in countries like Pakistan, there is limited specific data on the epidemiology and etiology of CP.3,4 CP predominantly affects males during the prenatal developmental period.5,6 Primarily, it manifests poor coordination, stiff or weak muscles, and tremors but can affect abilities to sense, see, hear, or speak. CP can be classified based on muscle tone, topographical distribution, severity, and Gross motor function classification system (GMFCS).1 Signs and symptoms vary from person to person based on the extent of the brain injury.
Functional limitations in CP-inflicted children are due to emotional, mental, physical, and social disorders1 which makes them fully or partially dependent on caregivers, especially mothers. They need external assistance for feeding, healthcare, personal care, and mobility. The dependency of a CP-inflicted patient has a direct influence on the economic, emotional, physical, and social wellbeing of the caregivers.7-9 Sometimes, taking care of disabled patients becomes a full-time occupation for the caregivers which puts them at risk of anxiety and depression.9 Studies from Brazil,10 Saudia Arabia,11 Turkey,12 and Zimbabwe13 observed that caregivers of CP children particularly mothers have higher levels of anxiety and depression than caregivers of healthy children. Research from Canada14 and Ireland15 has reported inferior physical and psychological well-being in caregivers of CP children.
In Pakistani society, often family members take care of patients by sacrificing their own physical and psychosocial well-being to provide extensive care to the patients. It is stressful for caregivers to balance the inevitable demands of CP-inflicted children and their own social needs which elicits several psychiatric problems. And, if the caregivers are unable to meet the challenges of caretaking due to psychiatric problems, their CP-inflicted child may not attain an optimal level of functioning. Everybody in Pakistan mostly overlooks the psychiatric problems among caregivers. It is important to consider the detrimental effects on the caregivers of CP-inflicted patients. There is a dearth of research in this context, especially in Pakistan. Limited studies have reported depression and anxiety levels among caregivers of children with CP and the results are controversial. The present study aimed to compare anxiety and depression among primary caregivers of male versus female children with cerebral palsy.
Methodology:
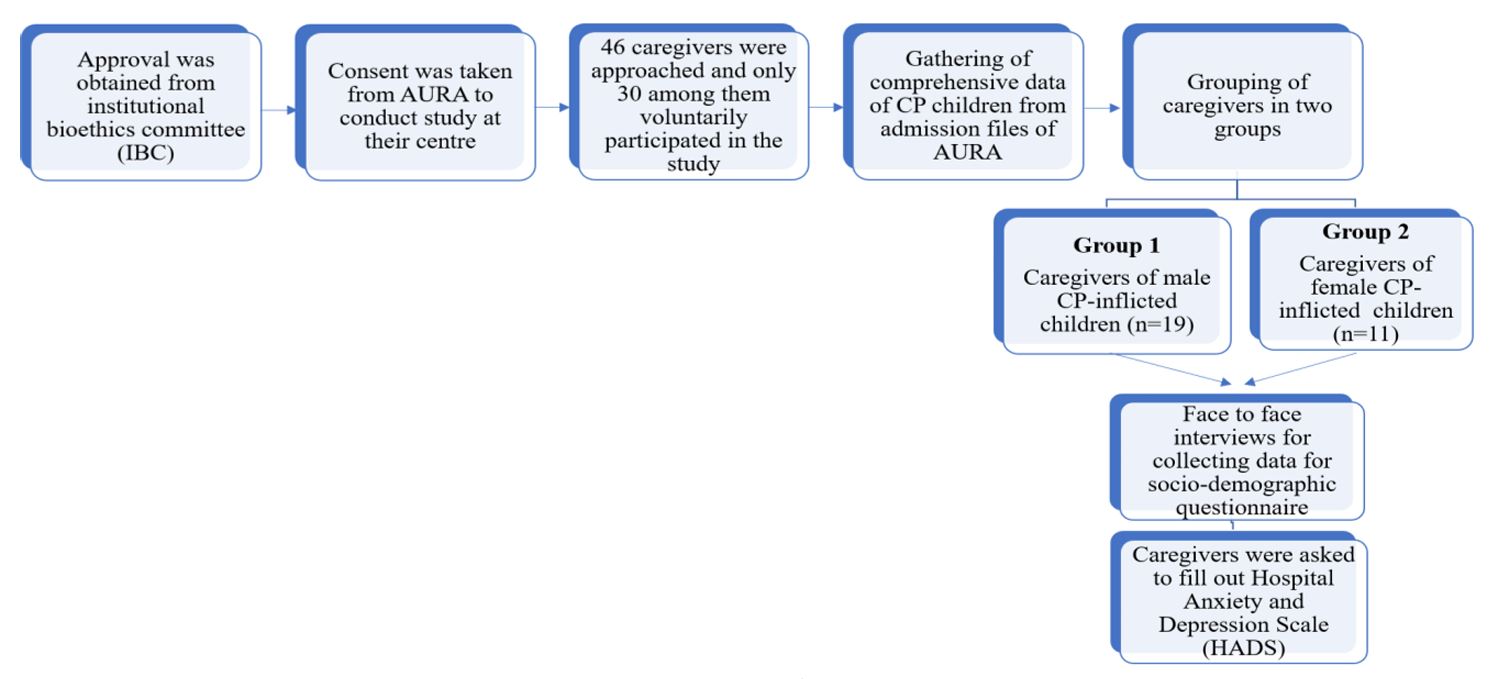
This cross-sectional comparative study was carried out between February 2020 and March 2021 with the caregivers of CP-inflicted children admitted at Al Umeed Rehabilitation Association, Karachi, Pakistan. Figure 1 shows the study protocol. Study approval was taken from the ‘Institutional Bioethics Committee’ of the University of Karachi (IBCKU-2017) followed by the permission of rehabilitation center. Written consent was also taken from the primary caregivers of CP children. Participants’ identities were kept confidential.
Primary caregivers living with CP child were included in the study. However, participants using any antidepressant or anxiolytic drugs and the absence of a history of psychological disorders were excluded
It was a 1st phase clinical study for which the sample size could be lower than twenty.16 The focus group was the caregivers of CP children. The caregivers were contacted by the rehabilitation center and their interviews were conducted in the presence of a psychologist within the premises of rehabilitation center. Among 46 approached caregivers, only 30 (75%) voluntarily participated in the present study. Group 1 encompassed caregivers of male (n=19) and group 2 encompassed caregivers of female CP-inflicted patients (n=11).
The present study involved 3 instruments including
- Characteristics of CP children: Age, gender, GMFCS, mobility, muscle tone, severity, topographical distribution, and presence of any additional impairments were recorded from the medical records at the center. Muscle tone was assessed using Modified Ashworth Scale (MAS) scale.
- Sociodemographic questionnaire for primary caregivers: 14-item questionnaire encompassing age, absence from work/commitments, blaming by people for a disabled child, district of residence, education, gender, income level, marital status, occupation, relationship with the child, religion, social support, and a total number of normal and disabled children.
- Anxiety and depression assessment among the primary caregivers: The Hospital Anxiety and Depression Scale (HADS) was designed by two scientists namely Snaith and Zigmond to provide clinicians with an adequate, valid, easily accessible, and reliable tool to assess anxiety and depression.17 HADS consists of fourteen questions with four response choices grouped into two subscales, anxiety (odd numbers) and depression (even numbers). The choices for each item are scored from zero to three for a total of twenty-one on each subscale. The cut-off point is the same for both anxiety and depression and is normal ‘0–7’; borderline abnormal ‘8–10’; or abnormal case ‘11 or more’. HADS has high reliability with a ‘0.84–0.87’ Cronbach alpha value and validity (p<0.05).17
Descriptive statistics were used to determine the frequencies, ratios, mean, and standard deviation of the acquired data. An independent t-test was employed to compare between-group differences for the primary caregivers of the male and female CP patients.
Figure 1: Flow chart for the study
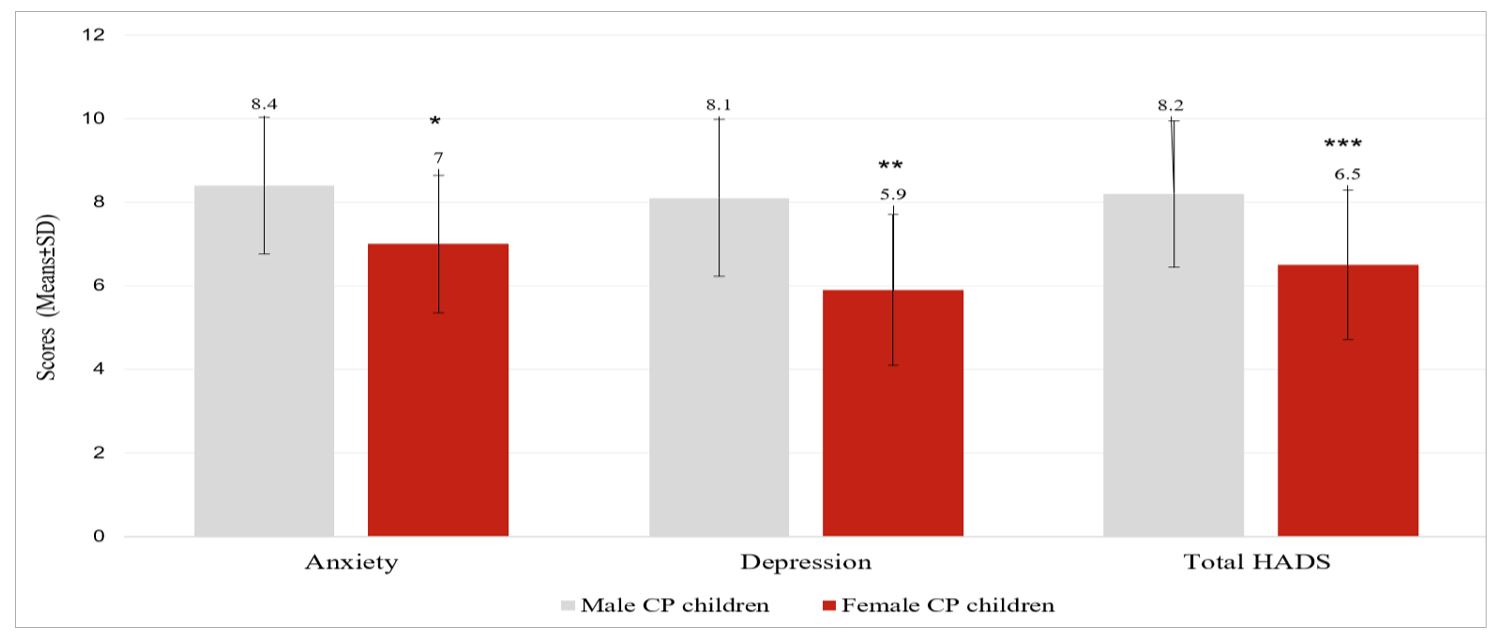
Figure 2: CP Child gender and anxiety, depression, and total HADS score of caregivers. Caregivers of male CP children compared with caregivers of female CP children. Values are significant at *p<0.05, **p<0.01, and ***p<0.001 (t-test). Error bars are Standard deviations.
Figure 2: Between Group Analysis among Male and Female CP Children
Results:
Characteristics of CP children: Table 1 presents the characteristics of CP children which encompassed 36.6% of females and 63.3% of males. The mean ages of male and female CP children were similar (14±4 years, and 14±4.6 years respectively). No significant differences were found between the two groups (p>0.05) (Table 1).
Sociodemographic questionnaire for primary caregivers: The mean age of primary caregivers in group 1 was 34.3±6.70 years and in group 2 was 34.2±6.57 years. Detailed sociodemographic data about the caregivers of both groups are given in Table 2.
Anxiety and depression assessment among the primary caregivers: Both groups showed anxiety and depression in the caregivers. Compared to the caregivers of female CP children, caregivers of male CP children had significantly higher anxiety (7.09±1.64; 8.42±1.6, p=0.044), depression (5.90±1.8; 8.10±1.88, p=0.004) and total HADS scores (6.50±1.79; 8.26±1.75, p=0.0006) (Figure 2).
A statistically significant difference was observed in the presence of additional impairments between the groups (p < 0.05) (Table 1). However, no significant differences were identified in the sociodemographic data of the caregivers between the two groups of children with cerebral palsy (p > 0.05) (Table 2).
| Table 1: Characteristics of CP children | |||||
| Category | Sub-category | Group 1
(n=19) |
Group 2
(n=11) |
Total
(n=30) |
p-value |
| Age (years) | Below 10 | 4 (21.0%) | 4 (36.3%) | 8 (26.6%) | 0.17 |
| 10–19 | 8 (42.1%) | 4 (36.3%) | 12 (40%) | ||
| 20–29 | 6 (31.5%) | 2 (18.1%) | 8 (26.6%) | ||
| 30–39 | 1 (5.26%) | 1 (9.09%) | 2 (6.66%) | ||
| ≥ 40 | 0 | 0 | 0 | ||
| GMFCS | Level I | 5 (26.3%) | 1 (9.09%) | 6 (20%) | 0.19 |
| Level II | 4 (21.0%) | 2 (18.1%) | 6 (20%) | ||
| Level III | 3 (15.7%) | 2 (18.1%) | 5 (16.6%) | ||
| Level IV | 7 (36.8%) | 4 (36.3%) | 11 (36.6%) | ||
| Level V | 0 | 2 (18.1%) | 2 (6.66%) | ||
| Muscle tone | Spastic | 11 (57.8%) | 4 (36.3%) | 15 (50%) | 0.40 |
| Hypotonic | 8 (42.1%) | 7 (63.6%) | 15 (50%) | ||
| Mobility | Independent | 5 (26.3%) | 1 (9.09%) | 6 (20%) | 0.18 |
| Walker | 5 (26.3%) | 1 (9.09%) | 6 (20%) | ||
| Wheelchair dependency | 9 (47.3%) | 9 (81.8%) | 18 (60%) | ||
| Severity | Mild | 5 (26.3%) | 1 (9.09%) | 6 (20%) | 0.09 |
| Moderate | 10 (52.6%) | 7 (63.6%) | 17 (56.6%) | ||
| Severe | 4 (21.0%) | 3 (27.2%) | 7 (23.3%) | ||
| Topographical distribution | Diplegia | 9 (47.3%) | 5 (45.4%) | 14 (46.6%) | 0.19 |
| Athetoid | 2 (10.5%) | 3 (27.2%) | 5 (16.6%) | ||
| Hemiplegia | 5 (26.3%) | 1 (9.09%) | 6 (20%) | ||
| Quadriplegia | 2 (10.5%) | 1 (9.09%) | 3 (10%) | ||
| Dystonia | 1 (5.26%) | 1 (9.09%) | 2 (6.66%) | ||
| Additional impairments | ADHD | 1 (5.26%) | 1 (9.09%) | 2 (6.66%) | 0.04 |
| Epilepsy | 3 (15.7%) | 1 (9.09%) | 4 (13.3%) | ||
| Intellectual disability | 2 (10.5%) | 2 (18.1%) | 4 (13.3%) | ||
| Poor attention | 5 (26.3%) | 2 (18.1%) | 7 (23.3%) | ||
| Incontinence | 4 (21.0%) | 3 (27.2%) | 7 (23.3%) | ||
| None | 4 (21.0%) | 2 (18.1%) | 6 (20%) | ||
| Values are frequencies and percentages. [ADHD; Attention Deficient Hyperactivity Disorder] | |||||
| Table 2: Sociodemographic data of each group of caregivers (n=30) | |||||
| Category | Sub-category | Group 1
(n=19) |
Group 2
(n=11) |
Total
(n=30) |
p-value |
| Age (Years) | Below 18 | 0 | 0 | 0 | 0.09 |
| 18-29 | 4 (21.0%) | 2 (18.1%) | 6 (20%) | ||
| 30-39 | 7 (36.8%) | 5 (45.4%) | 12 (40%) | ||
| 40-49 | 8 (42.1%) | 4 (36.3%) | 12 (40%) | ||
| ≥ 50 | 0 | 0 | 0 | ||
| Marital status | Never married | 1 (5.26%) | 0 | 1 (3.33%) | 0.38 |
| Married | 18 (94.7%) | 10 (90.9%) | 28 (93.3%) | ||
| Divorced | 0 | 0 | 0 | ||
| Separation | 0 | 0 | 0 | ||
| Widowed | 0 | 1 (9.09%) | 1 (3.33%) | ||
| Relationship of caregiver with the child | Father | 0 | 0 | 0 | 0.34 |
| Mother | 18 (94.7%) | 11 (100%) | 29 (96.6%) | ||
| Others | 1 (5.26%) | 0 | 10 (33.3%) | ||
| Religion | Islam | 18 (94.7%) | 11 (100%) | 29 (96.6%) | 0.34 |
| Christianity | 1 (5.26%) | 0 | 1 (3.33%) | ||
| Others | 0 | 0 | 0 | ||
| Education | None | 3 (15.7%) | 1 (9.09%) | 4 (13.3%) | 0.06 |
| Primary | 3 (15.7%) | 2 (18.1%) | 5 (16.6%) | ||
| Secondary | 6 (31.5%) | 5 (45.4%) | 11 (36.6%) | ||
| Higher | 7 (36.8%) | 3 (27.2%) | 10 (33.3%) | ||
| District of residence | East | 2 (10.5%) | 1 (9.09%) | 3 (10%) | 0.23 |
| West | 1 (5.26%) | 0 | 1 (3.33%) | ||
| South | 1 (5.26%) | 1 (9.09%) | 2 (6.66%) | ||
| Central | 13 (68.4%) | 7 (63.6%) | 20 (66.6%) | ||
| Malir | 0 | 1 (9.09%) | 1 (3.33%) | ||
| Korangi | 2 (10.5%) | 1 (9.09%) | 3 (10%) | ||
| Occupation | Housekeeping | 17 (89.4%) | 9 (81.8%) | 26 (86.6%) | 0.50 |
| Job | 2 (10.5%) | 2 (18.1%) | 4 (13.3%) | ||
| Income level of the family | Low | 0 | 0 | 0 | 0.42 |
| Middle | 19 (100%) | 11 (100%) | 30 (100%) | ||
| High | 0 | 0 | 0 | ||
| Presence of other child/children | Yes | 18 (94.7%) | 11 (100%) | 29 (96.6%) | 0.40 |
| No | 1 (5.26%) | 0 | 1 (3.33%) | ||
| Presence of any other disabled child | Yes | 0 | 0 | 0 | 0.50 |
| No | 19 (100%) | 11 (100%) | 30 (100%) | ||
| Social support to the caregiver | Yes | 15 (78.9%) | 9 (81.8%) | 24 (80%) | 0.29 |
| No | 4 (21.0%) | 2 (18.1%) | 6 (20%) | ||
| Absence from work/commitments due to caregiving | Yes | 2 (10.5%) | 2 (18.1%) | 4 (13.3%) | 0.50 |
| No | 17 (89.4%) | 9 (81.8%) | 26 (86.6%) | ||
| Been blamed for disabled child/children? | Yes | 1 (5.26%) | 1 (9.09%) | 2 (6.66%) | 0.50 |
| No | 18 (94.7%) | 10 (90.9%) | 28 (93.3%) | ||
| If blamed then, by whom? | Spouse | 0 | 0 | 0 | 0.39 |
| Immediate family | 1 (5.26%) | 0 | 0 | ||
| Others | 0 | 1 (9.09%) | 2 (6.66%) | ||
| None | 18 (94.7%) | 10 (90.9%) | 28 (93.3%) | ||
| Values are frequencies and percentages. | |||||
Discussion:
Findings demonstrated that the caregivers of male CP-inflicted children had significantly higher anxiety, depression, and total HADS scores as compared to the caregivers of female CP-inflicted children. Generally, the caregivers of children with disabilities experience greater anxiety and depression. In our comparative study, more serious cases of CP were observed in group 1 which might be the reason of 57.8% anxiety and 52.6% depression reported by the caregivers of the group. Wijesinghe et al. reported that male CP-inflicted children, with lower functional capacity, and lower socioeconomic level may increase the burden on the caregivers.18 In the present study, the children in Group 1 had 78.9% additional impairments which encompassed ADHD, epilepsy, intellectual disability, incontinence, and poor attention except for movement, and they may present in 25-80% of cases.19 Children with additional impairments are even more dependent on caregivers which may be one of the reasons for the higher reporting of anxiety and depression in the primary caregivers inducted in the present study. Seeking psychosocial interventions may reduce the burden on caregivers.20
Current findings indicate that anxiety, depression, and total HADS scores of male caregivers were significantly higher which is concordant with the findings of Al-Eithan and co-authors.11 The present study also showed that the primary caregivers were mothers of the children in both groups i.e., 29 (96.6%). Yilmaz and co-authors reported that mothers of CP-inflicted children have higher anxiety and depression which is concordant with the findings of the present study.12 There may be several reasons associated with the higher levels of anxiety and depression including lack of social support, low-income status, gender of primary caregiver, and the child’s intellectual disability as indicated in the present study.
The function of parents has a direct influence on the function of their CP-inflicted children.21 Several interventions can enhance functions in CP-inflicted patients including acupuncture, assistive devices, aqua therapy, behavior therapy, castings, chiropractic treatment, cognitive rehabilitation therapy, counseling, environmental enrichment techniques, hippotherapy, home programs, massage, medications, occupational therapy, parent training, physiotherapy, religion-based therapies, selective dorsal rhizotomy, sensory interventions, speech therapy, or even joint surgeries in extreme cases.22,23 To ensure the efficacy of interventions and to achieve the goals of maximizing child function, clinicians should also consider interventions to improve and support parent function, particularly their mental health.24 It has been reported that interventions likely cognitive-behavioral and psychoeducation are effective for the improvement of mental health in the caregivers of disabled children.25 The quality of life was not assessed in the present study, but caregiving has a significant impact on the quality of life of the mothers.26
The present study is the first in the literature that diagnosed and compared the levels of anxiety and depression among the caregivers of male and female CP-inflicted children in Karachi, Pakistan. The limitation of the study was the small sample size as a few caregivers gave consent. Another limitation of the study was the acquisition of data from a single rehabilitation center. More research with sufficient samples in multi-centers will further validate reported findings. However, further clinical studies with a larger sample size are required to identify anxiety and depression in the caregivers of CP children. More research on the identification and management of anxiety and depression in the caregivers of CP-inflicted children on a mass scale is necessary for Pakistan. It is essential to diagnose and develop adequate interventions as the foremost objective for minimizing the anxiety and depression problems of caregiving in Pakistan.
Conclusion:
It is concluded that caregivers of male CP children were more prone to anxiety, depression and total HADS. There was no significant correlation found between the sociodemographic profile of the caregivers and the characteristics of CP with the gender of CP children. Moreover, the present study indicated that caregivers of both groups had anxiety and depression.
Disclaimer
This research was presented at the ‘International Live Conference on Cerebral Palsy’ on the 17th of December 2022.
References:
- Palsi S, Bakıs G. Cerebral Palsy: An Overview. Prevention. Hamidiye Medical Journal. 2022; 3:1-6. doi: 10.4274/hamidiyemedj.galenos.2021.72792.
- McIntyre S, Goldsmith S, Webb A, Ehlinger V, Hollung SJ, McConnell K, et al. Global prevalence of cerebral palsy: A systematic analysis. Developmental Medicine & Child Neurology. 2022; 64:1494-506. doi: 10.1111/dmcn.15346.
- Rafique A. The burden of cerebral palsy in Pakistan: an insight into demographic and preventive plan. Cukurova Medical Journal. 2022; 47:1759-1760. doi:10.17826/cumj.1167076.
- Rafique A. An insight into the risk factors for cerebral palsy in Pakistan. Pakistan Journal of Public Health. 2022; 12:157. doi:10.32413/pjph. v12i4.1113.
- Rafique A. Gender-Based Variation in the Prevalence of Cerebral Palsy in Pakistan. Journal of Islamabad Medical & Dental College. 2024; 13:582-586. doi:10.35787/jimdc. v13i(Suppl.).1091.
- Rafique A. Etiological factors manifesting cerebralpalsy in Pakistan: A narrative review. Foundation University Journal of Rehabilitation Sciences. 2024; 4:119-124. doi:10.33897/fujrs. v4i2.390.
- Ones K, Yilmaz E, Cetinkaya B, Caglar N. Assessment of the quality of life of mothers of children with cerebral palsy (primary caregivers). Neurorehabilitation and Neural Repair. 19:232–237. doi: 10.1177/1545968305278857.
- Lee MH, Matthews AK, Park C. Determinants of health-related quality of life among mothers of children with cerebral palsy. Journal of pediatric nursing. 2019; 44:1-8. doi: 10.1016/j.pedn.2018.10.001.
- Terzi R. Musculoskeletal system pain and related factors in mothers of children with cerebral palsy. Agri. 2016; 28:18-24. doi: 10.5505/agri.2015.74436.
- Zanon MA, Batista NA. Quality of life and level of anxiety and depression in caregivers of children with cerebral palsy. Revista Paulista De Pediatria. 2012; 30:392-6. doi: 10.1590/S0103-05822012000300013.
- Al-Eithan MH, Robert AA, Al-Saeed AH. Mood problems of mothers with disabled children in Saudi Arabia. Saudi Medical Journal. 2010; 31:1161-5.
- Yilmaz H, Erkin G, Nalbant L. Depression and anxiety levels in mothers of children with cerebral palsy: a controlled study. European Journal of Physical and Rehabilitation Medicine. 2013; 49:823–7.
- Dambi JM, Jelsma J, Mlambo T. Caring for a child with cerebral Palsy: the experience of Zimbabwean mothers. African Journal of Disability. 2015; 4:168-72. doi: 10.4102/ajod. v4i1.168
- Brehaut JC, Kohen DE, Raina P, Walter SD, Russell DJ, et al. The health of primary caregivers of children with cerebral palsy: how does it compare with that of other Canadian caregivers? Pediatrics. 2004; 114:182-91. doi: 10.1542/peds.114.2. e182.
- Byrne MB, Hurley DA, Daly L, Cunningham CG. Health status of caregivers of children with cerebral palsy. Child: Care, Health and Development. 36:696–702. doi: 10.1111/j.1365-2214.2009.01047. x.
- Storer, B.E. Design and analysis of phase I clinical trials. Biometrics. 1989; 45:925-37.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica. 1983; 67:361-70. doi: 10.1111/j.1600-0447. 1983.tb09716. x.
- Wijesinghe CJ, Cunningham N, Fonseka P, Hewage CG, Ostbye T. Factors associated with caregiver burden among caregivers of children with cerebral palsy in Sri Lanka. Asia Pacific Journal of Public Health. 2015; 27:85-95. doi: 10.1177/1010539514548756.
- Odding E, Roebroeck ME, Stam HJ. The epidemiology of cerebral palsy: incidence, impairments and risk factors. Disability and Rehabilitation. 2006; 28:183-91. doi: 10.1080/09638280500158422.
- Gugala B, Penar-Zadarko B, Pięciak-Kotlarz D, Wardak K, Lewicka-Chomont A, Futyma-Ziaja M, et al. Assessment of Anxiety and Depression in Polish Primary Parental Caregivers of Children with Cerebral Palsy Compared to a Control Group, as well as Identification of Selected Predictors. International Journal of Environmental Research and Public Health. 2019; 16:4173. doi: 10.3390/ijerph16214173.
- Murphy N, Caplin DA, Christian BJ, Luther BL, Holobkov R, Young PC. The function of parents and their children with cerebral palsy. PM&R. 2011; 3:98-104. doi: 10.1016/j.pmrj.2010.11.006.
- Novak I, McIntyre S, Morgan C, Campbell L, Dark L, Morton N, et al. A systematic review of interventions for children with cerebral palsy: state of the evidence. Developmental Medicine & Child Neurology. 2013; 55:885–910. doi: 10.1111/dmcn.12246.
- Rehman A, Naz H, Rafique A. Effectiveness of environmental enrichment techniques on spastic diplegia and behavioral modulation of three cerebral palsy Pakistani children. Int J Sci Eng Res. 2019; 10:228-32.
- Murphy N, Caplin DA, Christian BJ, Luther BL, Holobkov R, Young PC. The function of parents and their children with cerebral palsy. PM&R. 2011; 3:98-104. doi: 10.1016/j.pmrj.2010.11.006.
- Bourke-Taylor HM, Lee DC, Tirlea L, Joyce K, Morgan P, Haines TP. Interventions to improve the mental health of mothers of children with a disability: Systematic review, meta-analysis and description of interventions. Journal of autism and developmental disorders. 2021; 51:3690-706. doi: 10.1007/s10803-020-04826-4.
- Sonune SP, Gaur AK, Shenoy A. Prevalence of depression and quality of life in primary caregiver of children with cerebral palsy. Journal of Family Medicine and Primary Care. 2021; 10:4205-11. doi: 10.4103/jfmpc.jfmpc_70_21.