Original Article: JRCRS.2025:13(3):153-159
6- Association between Smartphone Screen Time and Cervicogenic Headache Severity in Young Adults, a Cervical Flexion-Rotation Test-Based: A Cross-Sectional Study
Jannat Arshad1, Somia Faisal2, Nabeela Safdar3, Sahar Aslam4, Mishal Farwa5
1 Physical Therapist, Rehab Poly Clinic, Lahore, Pakistan
2 Physical Therapist, The Children’s Hospital, University of Child Health Sciences Lahore, Pakistan
3 Assistant Professor, Lahore University of Biological & Applied Sciences Lahore, Pakistan
4 Assistant Professor, Superior University Lahore, Pakistan
5 Physical Therapist, Rehab Poly Clinic, Lahore Pakistan
Full-Text PDF DOI: https://dx.doi.org/10.53389/JRCRS.2025130306
Abstract:
Background: With increased use of smartphones, extended screen time is associated with musculoskeletal disorders such as cervicogenic headaches. Poor postures and forward head posture can cause cervical spine dysfunction and result in headache. Young adults, especially students, are highly susceptible because of overuse of smartphones. The prevalence and severity of cervicogenic headaches in this population need to be identified for early treatment and prevention.
Objective: To determine the association between smartphone screen time and cervicogenic headache severity in young adults.
Methodology: This cross-sectional study was conducted on Doctor of Physical Therapy (DPT) students (n=175) using a non-probability convenience sampling technique. Participants included both male and female DPT students aged 18–25 years with more than three hours of daily smartphone screen time, while individuals with systemic diseases, whiplash injuries, psychiatric illnesses, or a history of cervical spine tumors were excluded. Cervicogenic headache severity was assessed using the Numeric Pain Rating Scale (NPRS), and cervical spine dysfunction was evaluated through the Cervical Flexion-Rotation Test (FRT).
Results: Of the 175 participants, 137 tested positive and 39 tested negatives on the Flexion Rotation Test (FRT). According to the NPRS (Numeric Pain Rating Scale), 35.4% of participants reported mild pain, 55.4% had moderate pain, and 9.1% experienced severe pain. Screen time and Cervicogenic Headache CGH pain severity were statistically significantly correlated, with a chi-square test value of 63.742 and a p-value of <0.001.
Conclusion: The majority of students experienced cervicogenic headaches associated with excessive smartphone use. Moreover, a statistically significant association was found between increased screen time and higher cervicogenic headache severity (χ² = 63.742, p <0.001), indicating that prolonged smartphone use may contribute to increased headache intensity in young adults.
Keywords: Cervicogenic Headache, Smartphone Addiction, Screen Time, Young Adult.
Introduction:
Cervicogenic headache (CGH) is a secondary headache that originates from cervical spine dysfunction, particularly the upper cervical vertebrae, associated muscles, joints, and neural structures.1 Pain typically initiates in the neck and radiates to the occipital and frontal regions of the head and exacerbates by neck movements.2 Patients frequently exhibit stiffness in their muscles, particularly in the levator scapulae, sternocleidomastoid, and upper trapezius, as well as decreased cervical mobility.3,4
The pathophysiology of CGH involves the convergence of the nociceptive afferents from the upper cervical spinal nerves (C1-C3) and the trigeminal nerve within the trigeminocervical nucleus, resulting in referred pain in the head.5 The anatomical structures involved are the C2-C3 intervertebral discs, upper cervical synovial joints, dura mater, and vascular elements such as the internal carotid artery.6,7 Poor posture, especially forward head posture, can contribute to CGH by increasing strain on cervical muscles and compromising motor control resulting in functional limitations.8
CGH pain is usually non-throbbing, originates in the upper neck, and radiates forward. It is frequently provoked by movements of the neck or trigger points in the muscles.9 Increased stiffness in the superficial neck muscles and weakness of the deep neck flexors are also linked to CGH.10 The pain process may also be exacerbated by inflammatory mediators such as nitric oxide and cytokines.11
Globally, headache disorders affect approximately 47% of the population, with CGH accounting for 15–20% of cases.12 The condition has been said to happen two to four times as frequently in women as men. However, it is often misdiagnosed as migraines or cluster headaches due to overlapping symptoms.13 Cervical spondylosis and other degenerative spinal changes may also contribute to CGH development.14
In recent years, excessive smartphone use has emerged as a major risk factor for musculoskeletal complaints, including CGH. Prolonged screen time often leads to poor posture and forward head positioning, which overloads cervical muscles and weakens deep neck flexors.15 Among young adults, especially students and heavy social media users, smartphone addiction rates range from 8.4% to 24.9% raising concerns about long-term spinal heath. 16,17
The Flexion-Rotation Test (FRT) is a valid tool for assessing upper cervical mobility, particularly at C1–C2 level, and is frequently used in CGH diagnosis.18 Headache severity is commonly measured using the Numeric Pain Rating Scale (NPRS), which ranges from 0 (no pain) to 10 (worst pain).19
Given the increasing reliance on smartphones among young adults, screen overuse has emerged as a potential contributor to musculoskeletal disorders, particularly cervicogenic headache (CGH). Despite its rising prevalence, the relationship between screen time and CGH severity remains underexplored. Investigating this link is important for identifying modifiable risk factors and guiding early prevention strategies. This study aims to determine the association between smartphone screen time and CGH severity in young adults, offering insights into the musculoskeletal impact of smartphone use and informing clinical and public health interventions.
Methodology
This cross-sectional study was conducted on Doctor of Physical Therapy (DPT) students at Lahore University of Applied Sciences (LUBAS) from September 2023 to January 2024. A non-probability convenience sampling technique was employed. The sample size was calculated using Taro Yamane’s formula, based on a population size of 311 DPT students enrolled in the Department of Physical Therapy at LUBAS. The calculated sample size (n = 175) was determined using 95% confidence level, with an anticipated population proportion (p = 0.05) and a precision level (d = 0.05). Ethical approval for this study was obtained from the Ethical Research Committee (ERC) of University of Biological and Applied Sciences under reference number DPT/ERB/19 on 20-09-2023.
Both male and female DPT students aged between 18-25 years with self-reported mobile phone screen time of more than three hours per day were included in the study. However, participants with any systemic disease, a history of whiplash injury, psychiatric illness or mental disorder, or tumors of the cervical spine were excluded. Informed consent was obtained from all participants before their inclusion in the study, and participation was entirely voluntary. Confidentiality of participant data was strictly maintained, and all communication was conducted with transparency.
The data was collected by a physical performance test which was Cervical Flexion Rotation Test (FRT) and pain was assessed by Numeric Pain Rating Scale (NPRS). FRT sensitivity and specificity were 92% (p <.001). The overall diagnostic accuracy was κ = 0.85 and 89% (p <0.001).20-22 Whereas, NPRS showed moderate reliability (ICC = 0.67).23
All collected data were entered and analyzed using the Statistical Package for Social Sciences (SPSS), version 26. Descriptive statistics such as frequencies, percentages, means, and standard deviations were used to summarize the data. The chi-square test was used to assess associations between categorical variables (e.g., screen time and CGH severity; gender and FRT outcomes). Spearman’s correlation was applied to determine the relationship between screen time and pain intensity. For comparison of pain intensity between male and female participants, an independent samples t-test was used. A p-value of less than 0.05 was considered statistically significant.
Results:
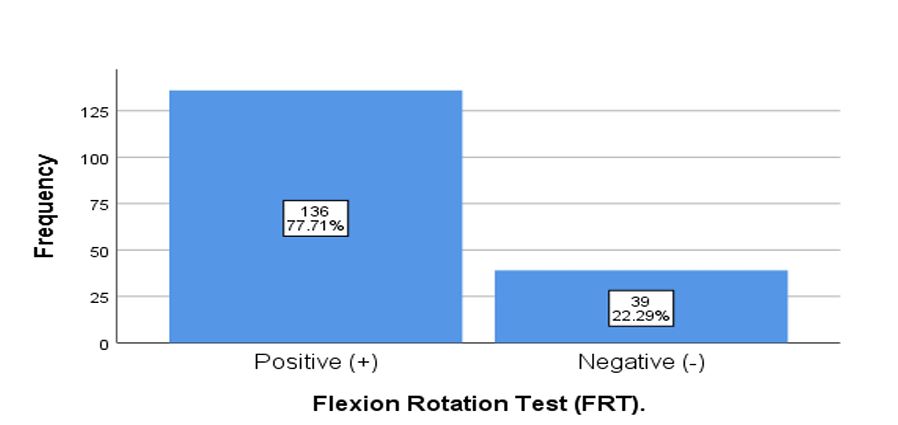
Out of the 175 participants (aged between 18 and 25 years), the mean age was 22.01 ± 2.29 years. Among them, 74 (42.3%) were male and 101 (57.7%) were female. Regarding screen time 48.6% (n= 85) of participants reported using their smartphones for 6–8 hours per day, while 44% (n=77) spent 4-6 hours and only 7.4% (n=13) used their phones for more than eight hours a day. Whereas, Flexion Rotation Test (FRT) was positive in 137 participants (77.7%) as shown in figure 1.
Figure 1: Bar-Chart showing frequency of Flexion Rotation Test
Figure 2: Pie-Chart showing the intensity of pain according to NPRS
Regarding pain intensity, most participants (56%, n=97) reported moderate pain, followed by mild pain (35%, n=62) and severe pain (9%, n=16), as shown in Figure 2. A statistically significant association was found between smartphone screen time and cervicogenic headache severity (χ² = 63.742, p <0.001; Table 1). Participants with mild pain primarily reported 4–6 hours of daily screen time, while those with moderate and severe pain increasingly reported longer screen exposure, with half of the severe cases using screens for more than 8 hours per day.
Spearman’s correlation coefficient (0.445) indicates a moderate positive association between smartphone screen time and pain intensity, with a statistically significant p-value of <0.001 as shown in table 2.
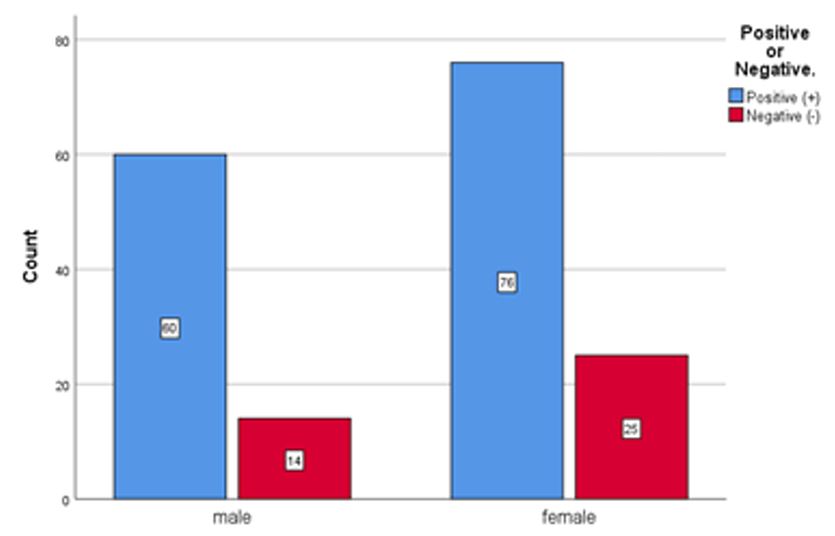
Table 3 represents the association between gender and FRT results. Among 175 participants, 136 (77.7%) tested positive, with 60 (44.1%) males and 76 (55.9%) females. There were 25 (64.1%) females and 14 (35.9%) males in the negative group. The chi-square test showed no statistically significant association between gender and FRT outcomes (p = 0.360).
Table 4 presents a comparison of pain intensity between male and female participants. Males (1.93 ± 0.67) reported a higher mean pain intensity than females (1.59 ± 0.53). An independent samples t-test showed a statistically significant difference between genders (t = 3.723, p < 0.001), with a mean difference of 0.338 (95% CI: 0.159–0.518).
An independent samples t-test was conducted to compare pain intensity between male and female participants, as the dependent variable (NPRS score) was continuous and the independent variable (gender) had two independent groups. Levene’s test confirmed the assumption of equal variances (F = 0.296, p = 0.587), thereby validating the use of the equal variances t-test. The results showed a statistically significant difference in pain intensity between genders (t = 3.723, df = 173, p <0.001), with males reporting higher mean pain scores (M = 1.93, SD = 0.67) compared to females (M = 1.59, SD = 0.53).
Figure 3: Bar Chart for CGH Prevalence and Severity by Gender
Figure 3 represents 60 (44.1%) males and 76 (55.9%) females had a positive FRT result. In contrast, 14 (35.9%) males and 25 (64.1%) females had a negative FRT result.
| Table 1: Association Between Screen Time and CGH Severity | ||||||
| Intensity of Pain | Screen Time Per Hour | Total | Chi-square | p-value | ||
| 4-6
hours |
6-8
hours |
>8
hours |
||||
| Mild (0-3) | 41 | 21 | 0 | 62 | 63.742a | <0.001 |
| Moderate (4-7) | 36 | 56 | 5 | 97 | ||
| Severe (8-10) | 0 | 8 | 8 | 16 | ||
| Total | 77 | 85 | 13 | 175 | ||
| a. 2 cells (22.2%) have expected count less than 5. The minimum expected count is 1.19. | ||||||
| Table 2: Spearman’s Correlation Between Smartphone Screen Time and Pain Intensity | ||
| Variable | Screen Time | Intensity of Pain |
| Spearman’s rho | 1.000 | 0.445** |
| Sig. (2-tailed) | – | <0.001 |
| N | 175 | 175 |
| **Correlation is significant at the 0.01 level (2-tailed). | ||
| Table 3: Association Between Gender and Flexion Rotation Test Results | |||||
| Gender | Flexion Rotation Test | Total | Chi-Square | p-value | |
| Positive (+ve) | Negative (-ve) | ||||
| Male | 60 (44.1%) | 14 (35.9%) | 74 (42.3%) | 0.839 a | 0.360 |
| Female | 76 (55.9%) | 25 (64.1%) | 101 (57.7%) | ||
| Total | 136 (100%) | 39 (100%) | 175 (100%) | ||
| a. 0 cells (0.0%) had an expected count less than 5. The minimum expected count was 16.49. | |||||
| Table 4: Comparison of Pain Intensity by Gender – Descriptive and Inferential Statistics | |||||||||
| Gender | N | Mean Pain Intensity | S. D | t-value | df | P-value | Mean Diff. | Std.
Error Diff. |
95% CI (Lower–Upper) |
| Male | 74 | 1.93 | 0.67 | ||||||
| Female | 101 | 1.59 | 0.53 | ||||||
| Comparison | 3.723 | 173 | <0.001 | 0.338 | 0.091 | 0.159 – 0.518 | |||
| Note: Levene’s Test for Equality of Variances: F = 0.296, p = 0.587 (equal variances assumed). | |||||||||
Discussion:
The purpose of this study was to determine the association between smartphone screen time and cervicogenic headache severity in young adults. According to the results, 77.7% of subjects had positive Flexion Rotation Test (FRT) results, suggesting that CGH is quite prevalent among smartphone users. Recent study showed a significant positive correlation between screen time and pain intensity, with a moderate correlation coefficient of 0.445 (p = 0.000). This suggests that as screen time increases, so does the intensity of pain. These findings support the link between extended smartphone usage and cervicogenic dysfunction, as demonstrated by a cross-sectional survey conducted by Aabrooi et al. (2022) that found 56% of students with cell phones had positive CFRT results.24
Javed et al. conducted a similar study to examine cervicogenic headache and neck pain in computer users. They found that 64.5% of people who used computers or laptops more than 3 hours had head and neck pain, with 40% indicating that their pain was between a 4 and a 6.25 This result is similar to that of the current study, in which 9.1% of participants reported severe pain (NPRS score of 8–10) while the majority (55.4%) reported moderate pain intensity (NPRS score of 4–7). These results are consistent, indicating that extended screen time whether from computers or smartphones plays a major role in cervicogenic headaches and neck pain.
A cross-sectional study conducted by Almutair et al. (2024) support recent research by showing how extended screen usage harms both visual and musculoskeletal health. According to their study, 79.5% of college students had neck pain, and a notable prevalence of visual disorders, such as nearsightedness (38%) and dry/itchy eyes (49%), which were reported by 62% of their participants. Whereas, there was a substantial correlation between higher neck impairment scores especially among female students and screen usage surpassing five hours.26 Likewise, current study revealed a favorable relationship between the amount of time spent on smartphones and the severity of discomfort.
Current study’s results are in contrast to those of Correia et al. (2021), who looked into the connection between adult neck pain and text neck. There was no significant correlation between the prevalence, frequency, or degree of neck discomfort and the cervical flexion angles during smartphone use (OR = 1.00; 95% CI: 0.98–1.02, p = 0.66 for standing, and OR = 0.99; 95% CI: 0.98–1.01, p = 0.93 for sitting).27 However, present study showed a somewhat positive relationship between screen time and pain intensity, with a Spearman’s rho of 0.445 (p = 0.000), indicating that more screen time is linked to more intense pain. Specifically, participants who used their smartphones for 6–8 hours reported moderate discomfort, whereas those who used them for more than 8 hours reported severe pain.
The association between office workers’ neck pain and excessive smartphone use was examined in a cross-sectional study by Nazi et al. (2021). According to the findings, neck pain was reported by 30.1% of participants, with a higher prevalence among females (33.3%) and younger workers (42.2 years). Notably, neck discomfort was six times more common in people with a smartphone overuse (SO) diagnosis (95% CI: 4.44–8.09, p < 0.001). Additionally, the study found a strong link between excessive smartphone use and psychological distress, such as melancholy, stress, and anxiety.28 These results are consistent with present study findings, which showed a substantial correlation between screen time and the intensity of cervicogenic headache (CGH). This suggests that extended screen time may make neck pain and related symptoms worse.
In a study conducted by Chen et al. (2021), the authors examined the relationship between screen time and musculoskeletal and visual discomfort among young smartphone users. The findings showed that all of the subjects reported experiencing visual discomfort, especially fatigued eyes. Furthermore, there was a positive correlation between screen time and eye strain (p < 0.05), with neck pain being the most important musculoskeletal symptom linked to prolonged screen use.29 These results are in line with current study’s findings, which further support the notion that extended screen time leads to musculoskeletal discomfort by showing a strong association between increased screen time and the intensity of neck pain.
There are several limitations to this study. The cross-sectional design restricts the ability to establish causality between screen time and musculoskeletal pain, while the reliance on self-reported screen time may introduce recall bias. Additionally, time constraints during data collection and low engagement from some participants during the Flexion Rotation Test (FRT) could have influenced the accuracy of results. The detailed explanation required for the FRT and Numeric Pain Rating Scale (NPRS) also prolonged the assessment process. Furthermore, the study sample was limited to students from Lahore University of Biological and Applied Sciences (LUBAS), which may affect the generalizability of findings.
Future research should consider randomized controlled trials (RCTs) to test the effectiveness of posture correction and screen-time reduction interventions in reducing cervicogenic headache severity. Additionally, longitudinal cohort studies involving larger and more diverse populations from different academic and occupational settings could help establish causal relationships. Incorporating objective screen time tracking tools (e.g., smartphone usage apps or wearable devices) and repeated clinical assessments such as the Flexion-Rotation Test (FRT) and muscle endurance measures would enhance data accuracy and reliability.
Conclusion
A significant association was found between increased smartphone screen time and the severity of cervicogenic headaches in young adults. Participants with prolonged daily screen exposure reported greater neck pain intensity and reduced cervical mobility, as assessed by the cervical flexion-rotation test. These findings highlight the need to monitor screen time and encourage ergonomic practices to prevent cervicogenic symptoms and promote cervical spine health in this population.
References:
- Patil Sr DS, Tikhile P, Gangwani N, Gangwani Jr N. Effectiveness of Nonpharmacological Measures on Improving Headache Score, Strength, Pain, and Quality of Life in Cervicogenic Headaches: A Systematic Review. Cureus. 2024 Mar 31;16(3).
- Piovesan EJ, Utiumi MA, Grossi DB. Cervicogenic headache–How to recognize and treat. Best Practice & Research Clinical Rheumatology. 2024 Feb 22:101931.
- Javed MT, Anam Abbas FA, Afzal R, Munir T, Azhar S. Cervicogenic Headache among Young Adults Using Computers with more than 3 Hours of Screen Time. PJMHS Vol15, No-12. 2021 Dec.
- Lu Z, Zou H, Zhao P, Wang J, Wang R. Myofascial Release for the Treatment of Tension‐Type, Cervicogenic Headache or Migraine: A Systematic Review and Meta‐Analysis. Pain Research and Management. 2024;2024(1):2042069.
- Sillevis R, Shamus E, Wyss K. Does Cervicogenic Headache Result in the Presence of Neural Tension, and Does this Affect the Position and Mobility of Atlas. Med. Clin. Res. 2021; 6:344.
- Demont A, Lafrance S, Gaska C, Kechichian A, Bourmaud A, Desmeules F. Efficacy of physiotherapy interventions for the management of adults with cervicogenic headache: A systematic review and meta‐analyses. PM&R. 2023 May;15(5):613-28.
- Jull G. Cervicogenic headache. Musculoskeletal Science and Practice. 2023 Aug 1; 66:102787.
- Pleș H, Florian IA, Timis TL, Covache-Busuioc RA, Glavan LA, Dumitrascu DI, Popa AA, Bordeianu A, Ciurea AV. Migraine: advances in the Pathogenesis and treatment. Neurology international. 2023 Sep;15(3):1052-105.
- Verma S, Tripathi M, Chandra PS. Cervicogenic headache: current perspectives. Neurology India. 2021 Mar 1;69(Suppl 1):S194-8.
- Lin LZ, Yu YN, Fan JC, Guo PW, Xia CF, Geng X, Zhang SY, Yuan XZ. Increased stiffness of the superficial cervical extensor muscles in patients with cervicogenic headache: A study using shear wave elastography. Frontiers in Neurology. 2022 May 27; 13:874643.
- Chowdhury SK, Zhou Y, Wan B, Reddy C, Zhang X. Neck strength and endurance and associated personal and work-related factors. Human factors. 2022 Sep;64(6):1013-26.
- Xu Y, Gao Y, Jiang L, Wu L, Yin J, Yang Z, Dong Y. Global trends in research on cervicogenic headache: a bibliometric analysis. Frontiers in Neurology. 2023 Apr 20; 14:1169477.
- Núñez‐Cabaleiro P, Leirós‐Rodríguez R. Effectiveness of manual therapy in the treatment of cervicogenic headache: A systematic review. Headache: The Journal of Head and Face Pain. 2022 Mar;62(3):271-83.
- Tu J, Vargas Castillo J, Das A, Diwan AD. Degenerative cervical myelopathy: insights into its pathobiology and molecular mechanisms. Journal of Clinical Medicine. 2021 Mar 15;10(6):1214.
- Halimah JA, Mojiri M, Hakami S, Mobarki O, Alanazi S, Alharbi A, Khalban F, Al Sheef A, Alnujaidi S, Almalawi M, Nasser F. Musculoskeletal health risks associated with smartphone use: a retrospective study from Riyadh, Saudi Arabia. Cureus. 2024 Jun 29;16(6).
- Wang Y, Kim YJ, Moon KA, Jeon HS. A Regression Analysis Study on the Presence of Pain in Specific Body Regions Based on Smartphone Usage Posture, Smartphone Addiction, Smartphone Usage Patterns. Physical Therapy Korea. 2024 Dec 20;31(3):250-61.
- Rękas M, Burzyńska J. Smart youth: sociodemographic factors, usage patterns, and self-reported vs. actual smartphone addiction among secondary school students. medRxiv. 2024 Apr 22:2024-04.
- Paquin JP, Dumas JP, Gérard T, Tousignant-Laflamme Y. A perspective on the use of the cervical flexion rotation test in the physical therapy management of cervicogenic headaches. Archives of Physiotherapy. 2022 Dec 8;12(1):26.
- Al-Khazali HM, Al-Sayegh Z, Younis S, Christensen RH, Ashina M, Schytz HW, Ashina S. Systematic review and meta-analysis of Neck Disability Index and Numeric Pain Rating Scale in patients with migraine and tension-type headache. Cephalalgia. 2024 Aug;44(8):03331024241274266.
- Hall TM, Robinson KW, Fujinawa O, Akasaka K, Pyne EA. Intertester reliability and diagnostic validity of the cervical flexion-rotation test. Journal of manipulative and physiological therapeutics. 2008 May 1;31(4):293-300.
- Anarte-Lazo E, Rodriguez-Blanco C, Bernal-Utrera C. Diagnostic accuracy of the flexion-rotation test and cut-off value in acute whiplash-associated disorders: A secondary analysis of a cross-sectional study1. Brazilian Journal of Physical Therapy. 2024 Nov 1;28(6):101134.
- Paquin JP, Dumas JP, Gérard T, Tousignant-Laflamme Y. A perspective on the use of the cervical flexion rotation test in the physical therapy management of cervicogenic headaches. Archives of Physiotherapy. 2022 Dec 8;12(1):26.
- Young IA, Dunning J, Butts R, Mourad F, Cleland JA. Reliability, construct validity, and responsiveness of the neck disability index and numeric pain rating scale in patients with mechanical neck pain without upper extremity symptoms. Physiotherapy theory and practice. 2019 Dec 2;35(12):1328-35.
- Aabroo S, Shafique S, Javed A, Fatima A, Khan O, Riaz S. Frequency of cervicogenic headache in students due to usage of smart devices–cross sectional survey. Pakistan Journal of Rehabilitation. 2022 Jul 7;11(2):39-44.
- Javed MT, Anam Abbas FA, Afzal R, Munir T, Azhar S. Cervicogenic Headache among Young Adults Using Computers with more than 3 Hours of Screen Time. PJMHS Vol15, No-12. 2021 Dec.
- Almutairi H, Alhammad L, Aldossari B, Alonazi A. Prevalence and Interrelationships of Screen Time, Visual Disorders, and Neck Pain Among University Students: A Cross-Sectional Study at Majmaah University. InHealthcare 2024 Oct 17 (Vol. 12, No. 20, p. 2067). MDPI.Correia IM, de Sá Ferreira A, Fernandez J, Reis FJ, Nogueira LA, Meziat-Filho N. Association between text neck and neck pain in adults. Spine. 2021 May 1;46(9):571-8.
- Derakhshanrad N, Yekaninejad MS, Mehrdad R, Saberi H. Neck pain associated with smartphone overuse: cross-sectional report of a cohort study among office workers. European Spine Journal. 2021 Feb; 30:461-7.
- Chen AH, Rosli SA, Basri R, Hoe CY. Investigation of screen time inclination and the accompanying visual and musculoskeletal discomfort in young smartphone users. Trends in Sciences. 2022 Jan 3;19(2):1753.