Original Article: JRCRS.2025:13(3):141-146
4- Immediate Effects of Taping on Patellofemoral Pain Syndrome in Outpatient Physical Therapy Patients at Rehman Medical Institute, Peshawar – Pre-Post Interventional Study
Rehana Nayab1, Mariyam Kifayat2, Shehla Nasir3, Farrakh Tariq4, Faizan Gohar5, Bilal Khan6
1 Senior Lecturer, Rehman College of Rehabilitation Sciences, Rehman Medical Institute (RMI), Peshawar, Pakistan
2 Lecturer, Rehman College of Rehabilitation Sciences, RMI, Peshawar, Pakistan
3 Intern Physical Therapy Department, Rehman College of Rehabilitation Sciences, RMI, Peshawar, Pakistan
4 Assistant Professor, Rehman College of Rehabilitation Sciences, RMI, Peshawar, Pakistan
5 Teaching Assistant, Rehman College of Rehabilitation Sciences, RMI, Peshawar, Pakistan
6 Assistant Professor / Principal, Rehman College of Rehabilitation Sciences, RMI, Peshawar, Pakistan
Full-Text PDF DOI: https://dx.doi.org/10.53389/JRCRS.2025130304
Abstract:
Background: Patellofemoral pain syndrome (PFPS) is one of the most common reasons for the development of knee joint pain usually over the anterior aspect and causes deterioration of the cartilage in between the superiorly lying patella and underneath femur. PFPS contributes to approximately 15-45% of diagnosed cases of knee pain among US population.
Objective: The objectives of this study were to evaluate immediate effects of taping on pain in patients with Patellofemoral Pain Syndrome and to determine the difference in responses according to gender, BMI, and the type of taping technique used.
Methodology: A total of 32 participants were recruited in this pre-post-interventional study. The participants were asked to descend a stair of 8-inch height before and after the application of tape and were asked to rate their pain from 1 to 10 while differences were recorded and analyzed.
Results: The results of the study indicated a statistically significant reduction in pain following the intervention, (p<0.05) with a post-intervention mean value of 3.5±1.7. There was no significant difference between based on the tapping technique. A significant difference between the BMI groups was observed, with individuals with normal BMI responding effectively towards treatment. There was no significant difference between the two gender groups, meaning that both genders respond equally towards treatment.
Conclusion: The results of this study show that short-term taping can significantly reduce knee pain in PFPS via sensory input, with BMI influencing pain relief, while gender and taping technique show no significant impact.
Keywords: Taping, Spider Taping, McConnell’s Taping, Tibial Internal Rotation Taping, Patella Femoral Pain Syndrome
Introduction:
The incidence of pain at the anterior side of knee is the most commonly encountered musculoskeletal complaints in both sports’ rehabilitation and general orthopedic practice. It amounts to a total of 22 cases per 1000 individuals annually.1 Among the many clinical presentations of anterior knee pain, Patellofemoral Pain Syndrome (PFPS) stands out as one of the most prevalent diagnoses, particularly in young, active populations. PFPS, often referred to as “runner’s knee,” can affect individuals across all levels of physical activity, from elite athletes to sedentary individuals, making it a significant concern for the general public.2 While structural causes such as overuse of knee extensors, osteochondral changes or patellar instability may contribute to this pain, most often the presenting cases are devoid of any structural deficits or arthrological manifestations.3 Typically, patients report diffused, poorly localized pain around or behind the patella, aggravated by activities that load the patellofemoral joint under flexion, such as stair climbing, running, squatting, or prolonged sitting with the knees bent also known as the ‘’theater sign’’.4 It is often characterized by retro-patellar pain brought on by weight bearing activities on flexed knee and palpation of the knee joint, while demonstrating negative results on the special tests for menisci, ligaments, bursae and plicae.5 PFPS is recognized as a multifactorial condition. The biomechanical contributors towards the condition include poor patellar tracking, quadriceps and hip muscle weakness, tight lateral structures, altered neuromuscular control, excessive foot pronation, and deficits in proprioception.6 Furthermore, some psychosocial factors such as catastrophizing the pain, fear-avoidance behaviors, and decreased self-efficacy can exacerbate symptoms of the condition and cause a major hindrance in the road to recovery from Patellofemoral Pain Syndrome.7 In the long run, if Patellofemoral Pain Syndrome is not managed promptly and properly, it can lead to long term consequences such as, gait disturbance, gradual reduction in physical activity levels, deconditioning and may also lead to early development of degenerative joint conditions.8 Various patient factors like gender, age, BMI etc. are also known to affect individual response to tape application which is the reason people respond in different ways to taping.9 Many treatment options are available for the management of Patellofemoral Pain Syndrome including therapeutic exercises for the hip and knee, gait retraining exercises, passive treatment approach such as patellar bracing and taping. Despite all these maneuvers, the condition is proven to have a higher rate of recurrence.10 Many studies have shown that patellar taping is a good adjunct for Patellofemoral Pain Syndrome along with gradually progressive therapeutic exercises. Among these techniques of patellar taping, the McConnell taping technique has gained considerable popularity due to its ability to provide immediate pain relief, correct abnormal patellar tracking, improve proprioceptive input, and facilitate optimal neuromuscular control.11
As the field of physical therapy continues to evolve locally, there is an increasing emphasis on patient-centered care, with a focus on rapid pain reduction to improve patient engagement and outcomes. Given the sociocultural importance of returning to daily activities quickly, especially in populations where prolonged rest is often not feasible, it is crucial to determine whether patellar taping can provide reliable, immediate relief of symptoms in this context. Despite the high prevalence and clinical significance of PFPS, there remains no single gold standard intervention. Physical therapy is the cornerstone of conservative management, typically involving exercise therapy, manual therapy, and adjunctive interventions such as taping. Patellar taping, specifically the McConnell taping technique, has been widely used in clinical practice to provide immediate pain relief, improve patellar alignment, enhance proprioception, and facilitate optimal muscle activation patterns. However, the evidence supporting the immediate effects of taping on pain reduction and functional improvement in diagnosed PFPS cases remains inconsistent and under-researched in local contexts. There is a significant gap in data from outpatient physical therapy departments in Pakistan, where variations in patient characteristics, therapist skills, and cultural factors may influence treatment outcomes. The results of this study do not only help quantify the short-term efficacy of taping in PFPS patients but also provide region-specific insights that can enhance clinical decision-making and evidence-based practice in musculoskeletal rehabilitation settings. This would lead to optimized treatment protocols, faster symptom relief, and improved patient satisfaction and would also help the future researchers to conduct their studies. The objectives of this study were to determine immediate effects of taping on pain in patients with Patellofemoral Pain Syndrome and to determine the difference in responses according to gender, BMI, and the type of taping technique used.
Methodology:
The study followed a pre-post interventional study design. It consisted of 32 participants. The sample was selected based on the number of patients presenting with complaints of knee pain for 3 months prior to the study. The study was carried out in the OPD of Physical Therapy and Rehabilitation Department, Rehman Medical Institute Peshawar from November 2022 to April 2023 with ethical approval from the department (with ref: 21-22/RMI/PT & Rehab Department/2023). The study included both male and female patients with diagnosed cases of Patellofemoral Joint Dysfunction with age ranging from 20-75 years. The researchers excluded those patients from the study who had a history of trauma to the lower limb, any infectious disease of the hip, knee or ankle that has occurred in the past 6 months, dislocation of patella in the past 6 months, were clinically diagnosed with arthritis or any musculoskeletal disease of the lower limb, had undergone knee surgery (TKA, Meniscal repair, Ligamentous reconstruction etc.) or had a clinically diagnosed neurological disease. Also, patients who had any clinically diagnosed dermatological disease were not recruited for the study as taping could have detrimental effects on already sensitized skin.
Patients visiting the OPD of Physical Therapy Department RMI for PFPS were voluntarily selected for the study. The participants were informed about the purpose and procedure of the study and consent was obtained. If the participant had PFPS in both knees, then the knee most painful was selected for the trial. The participants were asked to descend stairs with 8-inch height and were asked to rate their pain from 1 to 10 according to their perception. After this initial assessment, tape was applied, and the patients were asked to repeat the process. The patients were again asked their pain from 1 to 10 and differences were observed.
Rigid tape was applied to the participants by using three different techniques, i.e., McConnell taping, Spider taping or Tibial rotation taping.12 The patient’s rate of perceived pain was collected through Numeric Pain Rating Scale (NPRS).
Data was analyzed using SPSS version 22. Descriptive statistics were used to report gender, BMI and taping technique. Paired Sample t-test was used to analyze the difference between pre and post tape application pain levels. ANOVA was used to analyze the pain difference among BMI and taping technique. Independent sample t-test was used to analyze difference in pain between both male and female genders.
Results
Shapiro-Wilk test was applied to assess the normality of data. All variables had p-values greater than 0.05 with a confidence interval of 95%, which shows that the data was normally distributed.
Paired sample T-test was applied to determine the mean difference in pain scores before and after the application of tape. The results indicated a statistically significant reduction in pain following the intervention, (p<0.05) CI 95% (2.8,4.1), with a post-intervention mean value of 3.5±1.7. This suggests that taping is an effective intervention as there was a significant decrease in mean pain score after the intervention was applied.
To evaluate the differences among the 3 taping techniques, a one-way ANOVA was applied. The p-value obtained was greater than 0.05 CI 95% for difference between the groups, implying that there is no significant difference between the means of any of the pair. Thus, all the three taping techniques were equally effective in managing pain.
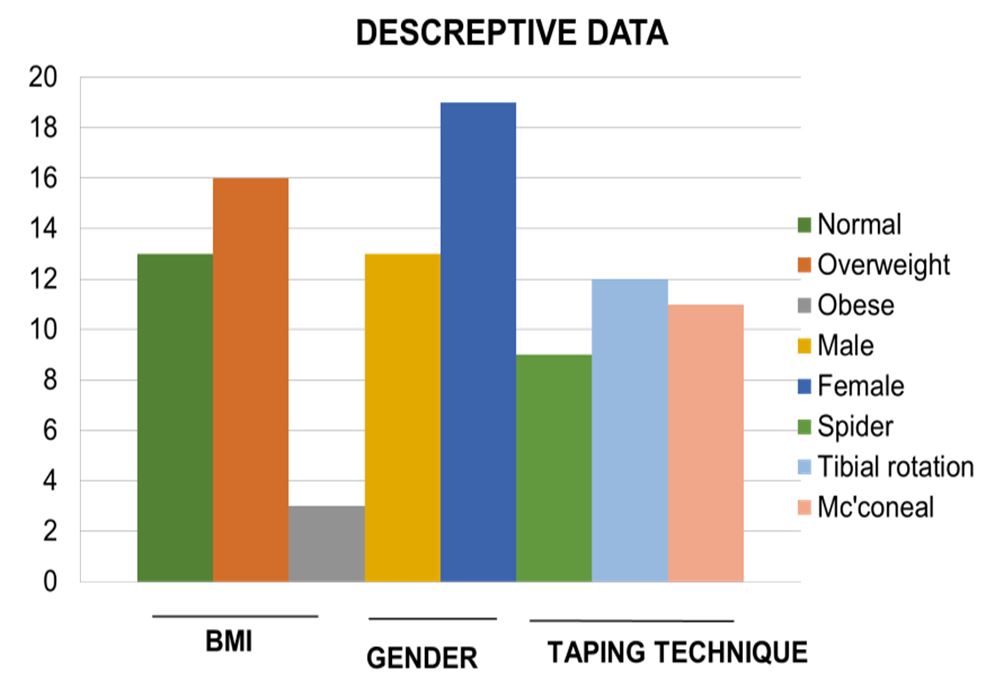
Figure 1: Descriptive statistics of the study, demonstrating the trends across BMI, gender and taping techniques.
| Table 1: Description of the p-values obtained by applying statistical tests with a CI of 95%. | ||
| Variable | Mean + SD | p-value |
| Normality of Data | Mean Pain Before Tape=7.69
Mean Pain After Tape=4.19 Pain difference= 3.5±1.7 |
0.3 |
| Difference before and after of tape application | Spider tape= 3.67± 1.5
Tibial Internal rotation tape= 3.83± 2.0 McConeal tape=3.09± 1.5 |
0.001 |
| Pain difference between the technique | Normal= 4.38 ± 1.8
Obese= 3.13 ± 1.4 Over-weight= 2.00 ± 0.0 |
0.58 |
| Pain difference between the BMI groups | Male= 4.00 ± 1.47
Female= 3.21 ± 1.84 |
0.034 |
| Pain difference between the Gender | Mean Pain Before Tape=7.69
Mean Pain After Tape=4.19 Pain difference= 3.5±1.7 |
0.233 |
Another one-way ANOVA was applied to determine pain difference between the three BMI categories. A significant p-value (<0.05) CI 95% indicated that BMI influenced pain outcomes between the groups. The mean pain difference was higher in the normal BMI group compared to that of obese (2.3) and overweight group (1.2), meaning that participants with normal BMI experienced greater reduction in pain after tape application. However, there is no significant difference between the obese and overweight group (-1.125). An Independent sample T-Test was applied to determine pain difference between the two genders. The p-value exceeded 0.05 CI 95% (-0.4,2.0), indicating no significant difference between males and females. Although the study consisted of 13 males and 19 females the results suggested that the intervention was equally effective, regardless of the gender.
Discussion
Taping is one of the widely accepted conservative management strategies used to alleviate pain and restore biomechanical alignment in individuals with Patellofemoral Pain Syndrome (PFPS). Our current study has shown a significant reduction in pain levels immediately after the application of taping, thus supporting its clinical utility in the symptomatic management of PFPS. The findings align with existing literature, emphasizing the immediate analgesic effects of taping and its role in optimizing lower limb biomechanics.13
A study published by Mao et. al.14 highlighted the importance of Kinesio taping for the treatment of Patellofemoral Pain Syndrome. The study concluded that while taping provided immediate pain relief, its effects were more visible when combined with a proper rehabilitation protocol, thus concluding that taping was more effective as an adjunct to therapeutic exercise and is not appropriate as an isolated treatment. However, the current study offers new insight by demonstrating that even as an isolated intervention, taping produced immediate reductions in pain intensity among participants. This suggests that in acute condition, or early rehabilitation phases, taping alone can provide valuable symptomatic relief when exercise is not immediately feasible.
A study by Dehghan et. al.,15 compared the levels of knee performance and pain in athletes suffering from Patellofemoral Pain Syndrome before and after tape application. The results demonstrated an increase in the repetition of step-down test along with an increase in bilateral squats post tape application. The present study also agrees with this as the participants were able to complete the step-down test along with a significant reduction in pain levels after the application of tape. These improvements may be the effect of enhanced proprioceptive feedback and altered neuromuscular control which is facilitated by the mechanical effects of the tape.
A systematic review conducted in Spain by Seijas et.al., 12 describes that tape application on a subject having Patellofemoral Pain Syndrome causes immediate decrease in the pain levels. However, the study has limited evidence regarding increase in long term functionality after the application of tape. The present study partially agrees with these results as the participants also experienced immediate decrease in pain levels after the tape was applied, without assessing long term outcomes.
A study conducted by Clifford et.al.,16 investigated the effects of McConnell’s taping technique and tibial internal rotation limitation technique on Single Leg Stance and lunge in patients suffering from Patellofemoral Pain Syndrome. The results of the study reported immediate reduction in pain and increase in functionality regardless of the type of tape applied. Similar to their results, the current study observed no substantial difference in pain reduction across different taping techniques, suggesting that the mechanical support and sensory input provided by the tape, rather than the specific method used, may be the key mediators of symptom relief.
Lee et.al.,17 demonstrated that Kinesio Taping improved proprioception and reduced patellofemoral joint stress during dynamic tasks, offering a potential mechanism for the immediate pain relief observed in their study. The present study also agrees with these findings as after the application of tape, functionality improved immediately and maybe attributed to the decrease in patellofemoral joint stress.
Chen et al.18 highlighted the importance of individualized taping strategies, showing that adapting taping techniques to each patient’s biomechanics produces better pain relief and standard outcomes. The current study applied a standardized taping protocol, but future research could explore whether personalized application techniques further enhance outcomes.
Thus, the findings of this study and the existing literature confirm that taping provides immediate and clinically meaningful reductions in pain among individuals with PFPS. While taping alone can offer short-term relief, it should ideally be used as a part of a comprehensive rehabilitation plan, incorporated into a comprehensive rehabilitation program that includes exercise therapy, biomechanical correction, and patient education.
Limitations: This study has several limitations that should be considered when interpreting the results. Power analysis was not performed and however considering the small sample size the findings may not be generalizable to a larger or more diverse populations. Only the immediate effects of taping were evaluated. Long-term outcomes such as sustained pain relief, functional improvements, or recurrence rates were not assessed. The study was conducted in one rehabilitation department (RMI Peshawar), limiting external validity across different clinical setups and populations. Both participants and researchers were aware of the intervention, which may have introduced performance or observer bias. While BMI, gender, and taping technique were analyzed, other factors such as physical activity level, muscle strength, and psychological factors were not controlled. The change in pain was assessed using NPRS only, without incorporating functional or quality-of-life outcomes.
Recommendations: Future research should recruit a larger sample size across multiple clinical settings to improve generalizability of the findings. Studies should investigate whether the pain relief achieved by taping is sustained over weeks or months, and whether it contributes to improved function and reduced recurrence. Incorporating randomization, control groups, and assessor blinding can reduce bias and strengthen the validity of results. In addition to pain, future studies should assess functional performance (e.g., step-down tests, squats, or gait analysis), quality of life, and patient satisfaction. Factors such as muscle strength, physical activity levels, foot biomechanics, and psychosocial influences should be examined to understand differential responses to taping. Research should compare standardized versus customized taping protocols based on patient-specific biomechanics to determine which yields better outcomes. Since taping alone offers only short-term relief, future studies should test its role as an adjunct to structured exercise programs and manual therapy for PFPS.
Conclusion
Numerous taping techniques may help people with PFPS in alleviating discomfort thereby facilitating rehabilitation exercise by healthcare professionals. Before the participants could acclimatize, the immediate sensory input provided by short-term application of tape may be sufficient to reduce knee discomfort abruptly through the modulation of afferent signals, which can help in inhibiting nociceptive pathways. BMI plays a significant influence on pain reduction achieved through taping suggesting that individuals falling into different BMI categories may respond differently to this treatment approach. However, the specific type of taping technique used, and the gender of the participants demonstrated that there was no statistically significant effect on pain outcomes, indicating that these factors may have a limited role in modulating the efficacy of taping interventions for PFPS.
References:
- Wilczyński B, Wąż P, Zorena K. Impact of three strengthening exercises on dynamic knee valgus and balance with poor knee control among young football players: A randomized controlled trial. Healthcare. 2021; 9(5):558.
- Lin I, Wiles L, Waller R, Goucke R, Nagree Y, Gibberd M, et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. British journal of sports medicine. 2020; 54(2):79-86.
- Souto LR, Silva DDO, Pazzinatto MF, Siqueira MS, Moreira RFC, Serrão FV. Are adjunct treatments effective in improving pain and function when added to exercise therapy in people with patellofemoral pain? A systematic review with meta-analysis and appraisal of the quality of interventions. British Journal of Sports Medicine. 2024; 58(14):792-804.
- Kakouris N, Yener N, Fong DT. A systematic review of running-related musculoskeletal injuries in runners. Journal of sport and health science. 2021; 10(5):513-22.
- Gant H, Ghimire N, Min K, Musa I, Ashraf M, Lawan A. Impact of the Quadriceps Angle on Health and Injury Risk in Female Athletes. International Journal of Environmental Research and Public Health. 2024; 21(12):1547.
- Duong V, Oo WM, Ding C, Culvenor AG, Hunter DJ. Evaluation and treatment of knee pain: a review. Jama. 2023; 330(16):1568-80.
- Willy RW, Hoglund LT, Barton CJ, Bolgla LA, Scalzitti DA, Logerstedt DS, et al. Patellofemoral pain: clinical practice guidelines linked to the international classification of functioning, disability and health from the academy of orthopaedic physical therapy of the American physical therapy association. Journal of Orthopaedic & Sports Physical Therapy. 2019; 49(9): CPG1-CPG95.
- Wang B, Mao Z, Guo J, Yang J, Zhang S. The non-invasive evaluation technique of patellofemoral joint stress: a systematic literature review. Frontiers in Bioengineering and Biotechnology. 2023; 11:1197014.
- Watson R, Sullivan B, Stone AV, Jacobs C, Malone T, Heebner N, et al. Lateral patellar dislocation: a critical review and update of evidence-based rehabilitation practice guidelines and expected outcomes. JBJS reviews. 2022; 10(5):e21.
- Pollatos D, Chandolias K, Giordamni M-A, Chalkia A, Trevlaki E. Review of new data in physiotherapeutic approach to Patellofemoral Pain Syndrome (PFPS). Journal of Biosciences and Medicines. 2021; 9(2):103-25.
- Skouras AZ, Kanellopoulos AK, Stasi S, Triantafyllou A, Koulouvaris P, Papagiannis G, et al. Clinical significance of the static and dynamic Q-angle. Cureus. 2022; 14(5).
- Seijas-Otero D, Alonso-Calvete A, Cuña-Carrera ID, Justo-Cousiño LA. Effects of taping in patellofemoral pain syndrome: A systematic review. Journal of back and musculoskeletal rehabilitation. 2023; 36(1):261-9.
- Wu H, Yao R, Wu J, Wen G, Wang Y. Does kinesio taping plus exercise improve pain and function in patients with knee osteoarthritis? A systematic review and meta-analysis of randomized controlled trials. Frontiers in Physiology. 2022; 13:961264.
- Mao H-Y, Hu M-T, Yen Y-Y, Lan S-J, Lee S-D. Kinesio taping relieves pain and improves isokinetic not isometric muscle strength in patients with knee osteoarthritis—a systematic review and meta-analysis. International journal of environmental research and public health. 2021; 18(19):10440.
- Dehghan F, Fouladi R, Martin J. Kinesio taping in sports: A scoping review. Journal of Bodywork and Movement Therapies. 2024; 40:1213-23.
- Clifford AM, Dillon S, Hartigan K, O’Leary H, Constantinou M. The effects of McConnell patellofemoral joint and tibial internal rotation limitation taping techniques in people with Patellofemoral pain syndrome. Gait & posture. 2020; 82:266-72.
- Lee JH, Rhim HC, Jang K-M. Effect of adding Kinesio Taping to exercise therapy in the treatment of patellofemoral pain syndrome. Medicina. 2023; 59(4):754.
- Luo Y, Chen X, Shen X, Chen L, Gong H. Effectiveness of Kinesio tape in the treatment of patients with patellofemoral pain syndrome: A systematic review and meta-analysis. Medicine. 2024; 103(23): e38438.