Original Article: JRCRS.2025:13(3):134-140
3- Comparison of Kinesiology Taping and Instrument Assisted Soft Tissue Mobilization in Cervicogenic Headache: A Randomized Clinical Trial
Sana Javaid1, Zainab Noor Qazi2, Mahnoor Zia3, Muhammad Ansar4
1 Consultant physical therapist, Healing Hands Mega Medical Complex Rawalpindi, Pakistan
2 Lecturer, Margalla Institute of Health Sciences, Rawalpindi, Pakistan
3 Student, Rawalpindi Medical College, Rawalpindi, Pakistan
4 Clinical Physiotherapist, Hamid Hospital, Rawalpindi, Pakistan
Full-Text PDF DOI: https://dx.doi.org/10.53389/JRCRS.2025130303
Abstract:
Background: Cervicogenic headache is a common condition caused by issue in the cervical spine, leading to chronic head pain. Various treatments exist, including kinesiology Taping and Instrument Assisted Soft Tissue Mobilization, but there is limited evidence comparing their effectiveness.
Objective: In this study, the effects of instrument-assisted soft tissue mobilization and kinesiology taping on pain severity, range of motion, and functional status in individuals with cervicogenic headache were compared.
Methodology: In the physiotherapy department of Healing Hands Institute, Mega Medical Complex, Rawalpindi, 36 participants with clinically diagnosed cervicogenic headache, headache, and stiffness in the neck, positive flexion rotation test with restriction of 6-10 degrees unilateral headache, aged 30-44 years, were divided into two equal groups for a clinical experiment that was randomized. While Group B received conventional therapy together with Instrument Assisted Soft Tissue Mobilizations (IASTM), Group A received conventional treatment along with Kinesiology Taping. Using a non-probability purposeful sampling approach, data was gathered at baseline and the fourth week to measure the indicator using the Numeric Pain Rating Scale, Neck Disability Index, and Bubble Inclinometer. SPSS version 22 was used for data analysis. (CTR : NCT05474612)
Results: At 4 weeks of intervention, both groups A and B saw substantial improvements in disability, range of motion, and discomfort (p < 0.05). Although there were no statistically significant differences in cervical flexion, extension, left lateral flexion, or left rotation (p > 0.05), between-group analysis revealed statistically significant differences in NPRS, NDI, cervical right rotation, and cervical right lateral flexion (p < 0.05). In the case of within-group comparisons, all measures showed statistically significant changes (p < 0.05).
Conclusion: The study concludes that the use of both instrument-assisted soft tissue mobilization and kinesiology taping has been successful in improving range of motion and lowering pain and impairment. However, Group B (Instrument Assisted Soft Tissue Mobilization) had a more notable improvement.
Keywords: Cervical Atlas, Cervicogenic Headache, Headache Unilateral, Mobilization, Range of Motion.
Introduction:
Chronic pain on one side of the head occurs as a result of anomalies in the cervical spine, such as intervertebral discs (C2-C3), synovial joints, upper cervical ligaments, suboccipital muscles, and C1-C2 nerve roots. The headache in the occipital area is also a result of the suboccipital nerves since they send branches to the at lanto-occipital joints.1 Even after the initial discomfort has subsided, persistent postural issues might exacerbate it by moving the neck or applying pressure to the back of the head.2 In 2004, the International Headache Society (IHS) defined persistent cervicogenic headache as pain that originates in the neck and radiates to the head or face. CEH may be influenced by the zygapophyseal joints of the cervical spine.3
The area around the head, neck, and shoulder muscles becomes more sensitive as a result of whiplash, strain, neck trauma, or continuous muscle spasm, similar to an allodynia situation seen in chronic migraine patients. Those who have a lower threshold for pain are more likely to have more severe symptoms.4 The pain can also be caused by the occipital nerves third and fourth (TON), along with the greater and lesser occipital nerves.5
Cervicogenic headache (CEH) is reported to have a prevalence of 4.1%. 6 Up to 20% of those who suffer from chronic or recurrent headaches are also affected by CEH, making it one of the most prevalent types of headache/condition. Four times as many women as men are affected by it.7
The three physical signs that can confirm the diagnosis of cervicogenic headache are decreased cervical extension range of motion, weak cervical muscles, and upper cervical joint dysfunction.8 The symptoms of CGH are numerous and include a one-sided headache, neck pain, whose severity increases during movements or abnormal body position, which induces pressure-related pain in the ipsilateral supero-posterior neck region, and neck, shoulder, or arm pain on the opposite side.9
Several types of spinal rehabilitation exercises may be done, including strengthening, stretching, and proprioceptive exercises. Screening for CEH through a physical examination is reliable and accurate.10
In early stages of treatment, neck traction and stretching are performed; in later stages, aerobic exercises and strength training are introduced according to patient condition and tolerance.11 Neck stiffness, headaches, and atrophy of profound cervical neck flexor muscles diminished when KT was utilized to treat mechanical neck issues.12
Instrument-Assisted Soft Tissue Mobilization (IASTM) is a novel and possibly useful treatment for fibrotic nodules, thickenings, ridges, adhesions, and scar tissue. IASTM can increase range of motion, decrease discomfort, and enhance overall function.20
Very little research has been done directly comparing the efficacy of kinesiology taping and instrument-assisted soft tissue mobilization (IASTM) in the treatment of cervicogenic headache (CH). However, existing studies suggest that IASTM is beneficial in alleviating various types of headaches and muscle soreness. Similarly, kinesiology taping has shown positive outcomes in addressing sports injuries, muscular imbalances, and improving pain and neuromuscular function. The possible advantages indicate that both methods have contributed to minimizing the pain, enhancing the range, and preventing disability among patients with cervicogenic headache.
Therefore, this study’s goal is to compare and evaluate the effectiveness of kinesiology taping and IASTM in treating cervicogenic headaches. This study may reveal important insights and therapeutic significance in both procedures, as no prior research has directly compared these two therapies for cervicogenic headache.
Therefore, this study will evaluate the efficacy of both interventions in pain, neck discomfort, and restricted range of motion in cervicogenic headache patients.
Methodology:
A Randomized Clinical Trial (RCT) with two groups—KT and IASTM—is used for this study. This trial was registered on www.clinicalTrials.com with registry number NCT05474612. The study was conducted at Healing Hands, Mega Medical Complex, Rawalpindi, for time duration of 3 months, i.e., from March 2022 to May 2022. Following approval by the RCR&AHS Institutional Review Board and Ethics Committee, the study got underway (with ref number: RIPHAH/FR&AHS/Letter-01313).
A sample size of 36 individuals (18 per group) with a 95 percent confidence level and an 80% power level was determined using the OpenEpi tool. This was using a mean difference between groups of 1 ( Group 1mean = 18.9, SD = 1; Group 2mean = 17.9, SD = 1) and revealed that 18 participants per group were sufficient to detect a clinically meaningful difference.13 The sample comprised participants, both males and females, 8 aged between 30-44 years with cervicogenic headaches, headache, and stiffness in the neck,14 positive flexion rotation test with restriction of 6-10 degrees, and unilateral headache with referred pattern. The study excluded participants with head and neck surgery, congenital deformities,15 erosive bone disorders, disc pathologies, neck infections and cancers, osteoarthritis, rheumatoid arthritis, and vertebral dislocation. 16 17
Following patient informed consent, a computerized random number generator was used to randomly assign the recruited individuals to Group A (KT) and Group B (IASTM) using the sealed envelope technique. The two groups were placed under the supervised treatment of 3 days weekly over 4 weeks. The recruitment process took place in a manner that preserved allocation concealment. Both were subjected to a total of 12 sessions. Group A (KT) was exposed to Kinesiology Taping, whereas Group B was subjected to instrument-assisted soft tissue Mobilization. At the start of therapy (baseline) and at the final session of the fourth week, data on outcome measures were collected. Both Groups A and B received conventional therapy that included stretching exercises of sternocleidomastoid, Upper fiber of trapezius, and Scalene and strengthening (isometric) of neck flexors (Longus capitis and Rectus capitis anterior).12, 18
Group A received conventional treatment with kinesiology taping. Kinesiology The upper trapezius fibers and the deep cervical extensor muscles (cervicis and semispinalis capitis) were taped. The distance between the occipital union and the T4/T5 vertebrae was measured in order to apply tape to the deep cervical extensors. Two Y-shaped strips of tape were attached along the spine, one on the right side and one on the left. The patients were then told to flex their necks as much as possible, and the tape was stretched. The tape’s base was attached at the T4 and T5 vertebrae, and an anchor was attached beneath the occipital union. Knuckles exerted pressure to improve its adherence. The distance between the acromion process and the occipital union was measured on the top fibers of the trapezius. Two pieces of tape were cut to the same length and affixed to the right and left sides, respectively. After instructing the patients to laterally flex their necks and fixing the tape’s base on the origin of the upper trapezius, an anchor was affixed to the acromion process at the point of insertion. Knuckles exerted pressure to stimulate the adhesive action.12, 19, 20 Kinesiology taping was applied on 1st session, and the patient was instructed to wear it for 2 days. Then, after a day’s gap next session was given, and the tape was changed, and so on.
Group B received conventional treatment along with the IASTM technique. As a result of IASTM’s ability to enhance blood, nutrition supply, and fibroblast migration to an injured location, these processes aid in the formation of extracellular matrix-like collagen, which in turn aids the healing process.21 As part of the treatment plan, IASTM was applied to the targeted muscles (SCM, the descending fiber of the trapezius, and the Sub occipitalis muscles (Rectus capitis posterior major, Rectus capitis posterior minor, Obliques capitis superior and inferior) in a comfortable position on the skin at 30° to 60° in a multidirectional stroking fashion for five minutes. Sweeping (effleurage strokes) lasts one minute, fanning (petrissage, or holding one end while moving the other in a semicircular pattern) lasts two minutes, and swiveling (rotating back and forth like manual compression with oscillation) lasts one minute. Both before and after the therapy session, the instrument was cleaned with alcohol sanitizer.22, 23
The Numeric Pain Rating Scale (ICC 0.67 [95 percent CI: 0.08–0.90] ) exhibits moderate reliability and was used to assess pain intensity.24 Disabilities were assessed using NDI, which shows excellent reliability (ICC = 0.88; [0.63 to 0.95]). 25 Inclinometer (ICC = 0.100, SEM = 1.39, P= 0.001) was used to assess Cervical range of motion.20, 26
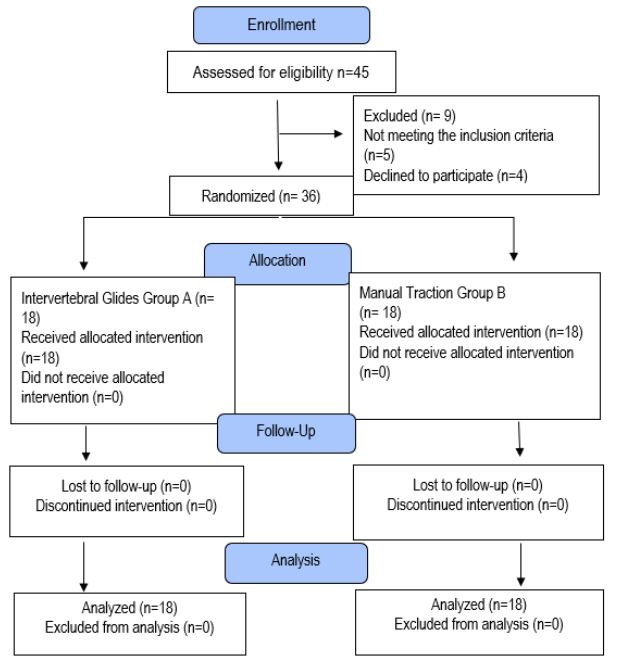
SPSS version 22 was used to analyze the data. Data were presented using the Consolidated Standards of Reporting Trials (CONSORT) checklist (Figure 1). Analytical analysis was based on normality testing for variables by the Shapiro–Wilk test as the sample size was less than 50. (Table 1) The majority of the eight variables were normally distributed because their p-value was greater than 0.05, and thus, parametric tests were used. Two variables were out of distribution because their p-value was less than 0.05, so these two variables were tested using non-parametric tests. Paired Sample T Test and Wilcoxon signed-rank test were used in doing the within-group analysis. Independent Sample T Test and Mann- Mann-Whitney U test was conducted to carry out the between-group analysis.
Figure 1: CONSORT Diagram showing Methodology
Results:
The results of the present study were described in tables and figures. The mean age was 36.39±4.14, with 30 years being the minimum age and 44 years being the maximum. Among 36 participants, 88.89% (n=32) were females and 11.11% (n=4) were males.
A Paired Sample T-test on the Neck Disability Index, Cervical Flexion, Cervical Extension, Right Lateral Flexion, Left Lateral Flexion, and Left Cervical Rotation was used to analyze Group A (Kinesiology taping) within the group. Right cervical rotation and NPRS were examined using the Wilcoxon signed-rank test. Group B (Instrument Assisted Soft Tissue Mobilization) underwent a Paired Sample T test, with all variables subjected to within-group analysis. Both Group A (kinesiology taping group) and Group B (IASTM group) had substantial modifications on all parameters, as evidenced by the findings, as given in Table 1 (p-value <0.001, i.e., p<0.05).
The Neck Disability Index, Cervical Flexion, Cervical Extension, Cervical Right Lateral Flexion, Cervical Left Lateral Flexion, and Cervical Left Rotation were all analyzed across groups using independent-T count. (Table 2) In the instance of right cervical rotation and NPRS, Mann-Whitney U was employed. While the p value for cervical flexion, cervical extension, cervical left lateral flexion, and cervical left rotation is (p >0.05), indicating that there is no statistically significant difference between the two groups, the results showed that the p value for NPRS, NDI, cervical right rotation, and cervical right lateral flexion is (p <0.05), indicating that the results are statistically very significant.
| Table 1: Within Group A Analysis (Paired Sample T test & Wilcoxon signed-rank Test) & Within Group B Analysis (Paired Sample T Test) | ||||||
| Within Group A Analysis (Paired Sample T test) | ||||||
| Variable | Mean ± S.D (PRE) | Mean ± S.D
(POST) |
p-value | |||
| NDI | 79.81±5.65 | 36.75±3.46 | <0.001 | |||
| Cervical Flexion | 60.11±3.71 | 67.83±4.27 | <0.001 | |||
| Cervical Extension | 56.72±4.38 | 62.66±4.08 | <0.001 | |||
| Cervical Right Lateral Flexion | 26.61±4.31 | 34.27±3.67 | <0.001 | |||
| Cervical Left Lateral Flexion | 25.44±3.64 | 36.4±4.03 | <0.001 | |||
| Cervical Left Rotation | 73.00±4.93 | 80.50±2.97 | <0.001 | |||
| Within Group B Analysis (Paired Sample T test) | ||||||
| Variable | Mean ± S.D (PRE) | Mean ± S.D
(POST) |
p-value | |||
| NPRS | 7.17±1.09 | 3.33±0.97 | <0.001 | |||
| NDI | 81.60±8.02 | 27.90±3.34 | <0.001 | |||
| Cervical flexion | 63.11±5.78 | 77.72±4.16 | <0.001 | |||
| Cervical extension | 57.05±3.78 | 65.61±1.91 | <0.001 | |||
| Cervical Right Lateral Flexion | 31.72±3.59 | 40.27±2.27 | <0.001 | |||
| Cervical Left Lateral Flexion | 31.38±4.96 | 40.44±2.73 | <0.001 | |||
| Cervical Right Rotation | 73.55±5.38 | 83.05 ±3.49 | <0.001 | |||
| Cervical Left Rotation | 73.94±5.10 | 83.05±3.37 | <0.001 | |||
| Within Group A Analysis (Wilcoxon signed Rank test) | ||||||
| Variable | Assessment | Median
(IQR) |
Mean ± S.D | z value | p-value | |
| NPRS | Pre-Treatment | 7(2) | 7.05±8.93 | -3.794 | <0.001 | |
| Post Treatment | 4(1) | 4.16±0.857 | ||||
| Cervical Right Rotation | Pre-Treatment | 75(6) | 74.27±4.19 | -3.742 | <0.001 | |
| Post Treatment | 80(4) | 80.44±3.07 | ||||
| Table 2: Between-group Comparison (Independent sampled T Test) | ||||
| Variables | Kinesiology Taping Group Mean ± S.D | IASTM Group Mean ± S.D | p-value | |
| NDI | Pre | 79.81±5.65 | 81.60±8.02 | 0.444 |
| Post | 36.75±3.13 | 27.90±3.34 | <0.001 | |
| Cervical Flexion | Pre | 60.11±3.71 | 63.11±5.78 | 0.085 |
| Post | 67.83±4.27 | 77.72±4.15 | 0.795 | |
| Cervical Extension | Pre | 56.72±4.38 | 57.05±3.78 | 0.305 |
| Post | 62.66±4.09 | 65.61±1.91 | 0.069 | |
| Cervical Right Lateral Flexion | Pre | 26.61±4.31 | 31.72±3.59 | 0.118 |
| Post | 34.27±3.68 | 40.27±2.27 | 0.043 | |
| Cervical Left Lateral Flexion | Pre | 25.44±3.65 | 31.38±4.96 | 0.420 |
| Post | 34.05±4.03 | 40.44±2.73 | 0.148 | |
| Cervical Left Rotation | Pre | 73.00±4.93 | 73.94±5.10 | 0.869 |
| Post | 80.50±2.98 | 83.05±3.37 | 0.386 | |
| Table 3: Between-Group Comparison (Mann-Whitney U Test) | |||||||||
| Variables | Median (IQR) KT | Median (IQR)
IASTM |
Mean±S.D
KT |
Mean±S.D
(IASTM) |
Mean Rank (Sum of Rank) Kinesiology Taping Group | Mean Rank (Sum of Rank) IASTM Group | U value | p- value | |
| NPRS | Pre | 7(2) | 7(2) | 7.06±0.938 | 7.17±1.098 | 17.86(321.50) | 19.14(344.50) | 150.50 | 0.704 |
| Post | 4(1) | 4(1) | 4.17±0.857 | 3.33±0.970 | 22.78(410.00) | 14.22(256.00) | 85.00 | 0.011 | |
| Cervical Right Rotation | Pre | 74(6) | 74(6) | 74.27±4.19 | 73.55±5.38 | 19.81(356.50) | 17.19(309.50) | 138.50 | 0.455 |
| Post | 82(5) | 83(5) | 80.44±3.07 | 83.05±3.48 | 14.33(258.00) | 22.67(408.00) | 87.00 | 0.017 | |
Figure 2: Kinesiology Taping and Instrument Assisted Soft Tissue Mobilization application
Discussion
Cervicogenic headache is a worldwide burden in the healthcare system, affecting the quality of life of many people without them knowing they have this condition. We conducted our study to determine the effects of kinesiology taping and instrument-assisted soft tissue mobilization on the parameters of pain type (pain intensity), cervical range of motion, and impairment in individuals with cervicogenic headache. This has been analyzed in previous literature is the impact of IASTM and kinesiology tape on cervicogenic, but this paper offers a new comparison between the two groups. According to the findings of this study, which were based on earlier research by Veena Kirthika et al. in 2021 to compare the effectiveness of kinesiology taping, trigger point therapy, and Mulligan sustained natural apophyseal glides for the treatment of cervicogenic headaches, the groups’ mean values for the Visual Analogue Scale and Cervical Extension range of motion showed a significant improvement in the post-test mean values.27 Another study by Mr. Rohit Banerjee et al. in 2021 evaluated the effectiveness of the instrument-assisted soft tissue mobilization technique on cervicogenic headache in college students addicted to smartphones. They found that IASTM is an effective intervention for the treatment of disability and the release of myofascial trigger points associated with patients with cervicogenic headache. This is consistent with our study’s findings that the use of IASTM stimulates connective tissue remodeling, as well as inducing collagen regeneration and repair and fibroblast recruitment that leads to the breakdown of scar tissue, improves fascial restrictions, and releases adhesions, which reduces pain 23 Zabih Allah Rasti et al. carried out research in 2019 to ascertain the immediate and long-term impacts of kinesiology tape on myofascial pain syndrome patients’ pain, range of motion, and disability. Applying kinesiology therapy has a considerable impact on pain, range of motion, and impairment, according to all metrics. This study’s results are consistent with ours since, following four weeks of Kinesio taping treatment, post-p-values indicated a substantial improvement in pain NPRS, cervical flexion, extension, lateral flexion, and rotation.28.
A limitation of this research is that p-values have been used to determine statistical significance, but the effect size (i.e., Cohen’s d or partial eta squared) was not computed. Post hoc analysis was not computed (such as Bonferroni or Holm-Bonferroni) applied for multiple comparisons. Although the study used a sealed envelope method to carry out randomization and allocation concealment during recruitment, there was no baseline comparison between groups to indicate how effective the randomization had been. Future research ought to consider measuring effect sizes, implementing adjustments for multiple comparisons, and reporting baseline group characteristics.
Conclusion
The research concluded that both Kinesiology Taping and Instrument Assisted Soft Tissue Mobilization procedures are effective in reducing pain and disability, and an increase in the range of mobility. Nevertheless, Group B (Instrument Assisted Soft Tissue Mobilization) demonstrated significant improvement.
References
- Park SK, Yang DJ, Kim JH, Kang DH, Park SH, Yoon JHJJopts. Effects of cervical stretching and cranio-cervical flexion exercises on cervical muscle characteristics and posture of patients with cervicogenic headache. 2017;29(10):1836-40.
- Uthaikhup S, Barbero M, Falla D, Sremakaew M, Tanrprawate S, Nudsasarn AJPM. Profiling the extent and location of pain in migraine and cervicogenic headache: a cross-sectional single-site observational study. 2020;21(12):3512-21.
- Mohamed AA, Shendy WS, Semary M, Mourad HS, Battecha KH, Soliman ES, et al. Combined use of cervical headache snag and cervical snag half rotation techniques in the treatment of cervicogenic headache. 2019;31(4):376-81.
- Al Khalili Y, Ly N, Murphy PB. Cervicogenic headache. 2018.
- Grandhi RK, Kaye AD, Abd-Elsayed AJCP, Reports H. Systematic review of radiofrequency ablation and pulsed radiofrequency for management of cervicogenic headaches. 2018;22(3):1-9.
- Haas M, Bronfort G, Evans R, Schulz C, Vavrek D, Takaki L, et al. Dose-response and efficacy of spinal manipulation for care of cervicogenic headache: a dual-center randomized controlled trial. 2018;18(10):1741-54.
- Garcia JD, Arnold S, Tetley K, Voight K, Frank RAJFin. Mobilization and manipulation of the cervical spine in patients with cervicogenic headache: any scientific evidence? 2016; 7:40.
- Getsoian SL, Gulati SM, Okpareke I, Nee RJ, Jull GAJBo. Validation of a clinical examination to differentiate a cervicogenic source of headache: a diagnostic prediction model using controlled diagnostic blocks. 2020;10(5): e035245.
- Howard PD, Behrns W, Martino MD, DiMambro A, McIntyre K, Shurer CJJoM, et al. Manual examination in the diagnosis of cervicogenic headache: a systematic literature review. 2015;23(4):210-8.
- Haas M, Brønfort G, Evans RL, Leininger B, Schmitt J, Levin M, et al. Spinal rehabilitative exercise or manual treatment for the prevention of cervicogenic headache in adults. 2017;2017(7).
- Xiao H, Peng B, Ma K, Huang D, Liu X, Lu Y, et al. The Chinese Association for the Study of Pain (CASP): Expert Consensus on the Cervicogenic Headache. 2019;2019.
- Neyazi LA, Fayaz NA, Zahran SSA, Azzam AHJTEJoHM. The Effect of Adding Kinesio Tape to Mulligan’s Mobilization in Patients with A Cervicogenic Headache. 2020;81(5):2063-8.
- Park SK, Yang DJ, Kim JH, Heo JW, Park SH, Uhm YH, et al. Effects of cranio-cervical flexion with transcranial direct current stimulation on muscle activity and neck functions in patients with cervicogenic headache. Journal of Physical Therapy Science. 2019;31(1):24-8.
- Nambi S, Pancholi D, Trivedi P, Momin S, Patel SJIJPSM. Comparative effect between C1-C2 self-sustained natural apophyseal glide (SNAG) and deep cervical flexors strength training in the management of cervicogenic headache. 2014;4(2):69-73.
- Patra RC, Mohanty P, Gautam APJAJPCR. Effectiveness of C1-C2 sustained natural apophyseal glide combined with dry needling on pressure point threshold and headache disability in cervicogenic headache. 2018;11(1):171-4.
- Saleh HM, Edward MOF, Fattah AAFA, Ali MFJTEJoO. Potentiation of physiotherapy by low-level laser or kinesio taping for treatment of cervicogenic headache: a randomized controlled study. 2016;32(4):248-54.
- National Library of Medicine NCfBI-N. [Available from: https://clinicaltrials.gov.
- Ay S, Konak HE, Evcik D, Kibar SJRbdr. The effectiveness of Kinesio Taping on pain and disability in cervical myofascial pain syndrome. 2017; 57:93-9.
- Neyazi LA, Fayaz NA, Zahran SSA, Azzam AH. The Effect of Adding Kinesio Tape to Mulligan’s Mobilization in Patients with A Cervicogenic Headache. The Egyptian Journal of Hospital Medicine. 2020;81(5):2063-8.
- Saleh HM, Edward MOF, Fattah AAFA, Ali MF. Potentiation of physiotherapy by low-level laser or kinesio taping for treatment of cervicogenic headache: a randomized controlled study. The Egyptian Journal of Otolaryngology. 2016;32(4):248-54.
- Kim J, Sung DJ, Lee JJJoer. Therapeutic effectiveness of instrument-assisted soft tissue mobilization for soft tissue injury: mechanisms and practical application. 2017;13(1):12.
- Banerjee R. Effectiveness of Instrument Assisted Soft Tissue Mobilisation Technique on Cervicogenic Headache in Smartphone Addicted College Students: A Pilot Study. 2021.
- Banerjee R. Effectiveness of instrument assisted soft tissue mobilisation technique on cervicogenic headache in smartphone addicted college students: a randomized clinical trial. International Journal of Research and Analytical Reviews (IJRAR). 2022.
- Lerner-Lentz A, O’Halloran B, Donaldson M, Cleland JAJJoM, Therapy M. Pragmatic application of manipulation versus mobilization to the upper segments of the cervical spine plus exercise for treatment of cervicogenic headache: a randomized clinical trial. 2021;29(5):267-75.
- Young IA, Dunning J, Butts R, Cleland JA, Fernández-de-Las-Peñas CJC. Psychometric properties of the Numeric Pain Rating Scale and Neck Disability Index in patients with cervicogenic headache. 2019;39(1):44-51.
- Ozdemir C, Kabuk A. The effects of profession‐related films on the professional pride of nursing students: A randomised controlled trial. Nursing Open. 2024;11(8): e70000.
- Kirthika VS, Kowsalya J, Padmanabhan K, Paul J, Sudhakar S, Kumar MG, et al. Efficacy of three different conservative interventions in the management of cervicogenic headache. Research Journal of Pharmacy and Technology. 2021;14(2):1094-8.
- Rasti ZA, Shamsoddini A. The short-term and long-term effects of kinesio taping on pain, range of motion and disability of neck in patients with myofascial pain syndrome: a randomized clinical trial. Trauma Monthly. 2018;24(1):1-6.
| Copyright Policy
All Articles are made available under a Creative Commons “Attribution-NonCommercial 4.0 International” license. (https://creativecommons.org/licenses/by-nc/4.0/). Copyrights on any open access article published by Journal Riphah college of Rehabilitation Science (JRCRS) are retained by the author(s). Authors retain the rights of free downloading/unlimited e-print of full text and sharing/disseminating the article without any restriction, by any means; provided the article is correctly cited. JRCRS does not allow commercial use of the articles published. All articles published represent the view of the authors and do not reflect the official policy of JRCRS. |