Original Article: JRCRS.2025:13(3):126- 133
2- Comparing Neuromuscular Training and Closed Chain Exercises in Athletes with Ankle Sprains: Efficacy in Pain Reduction, Joint Mobility, Balance, And Functional Disability: A Randomized Control Trial
Aamir Gul Memon1, 2, Suriyakala Perumal Chandran3, Abdul Hameed4, Shahzaib Saleem5, Ali Sheraz6
1 PhD (Scholar), Lincoln University College Malaysia
2 School of Basic Medical Sciences, Shandong University China
3 Assistant Professor/Deputy Dean MD Pre- Clinical, Lincoln University College, Malaysia
4 5 Lecturer Physical Therapy Department, Suleman Roshan Medical College, Tando Adam, Pakistan
6 MSc High Performance Sports Student, University of Saarland, Germany
Full-Text PDF DOI: https://dx.doi.org/10.53389/JRCRS.2025130302
Abstract:
Background: Ankle sprains are one of the most common musculoskeletal injuries in athletes and are caused mainly by inversion during dynamic movement, change of direction, and jump. The injuries predominantly affect the lateral ligament complex, with emphasis on the anterior talofibular ligament
Objective: To determine the effects of neuromuscular training versus closed kinetic exercise on pain, range of motion, balance, and function in athletes with ankle sprain.
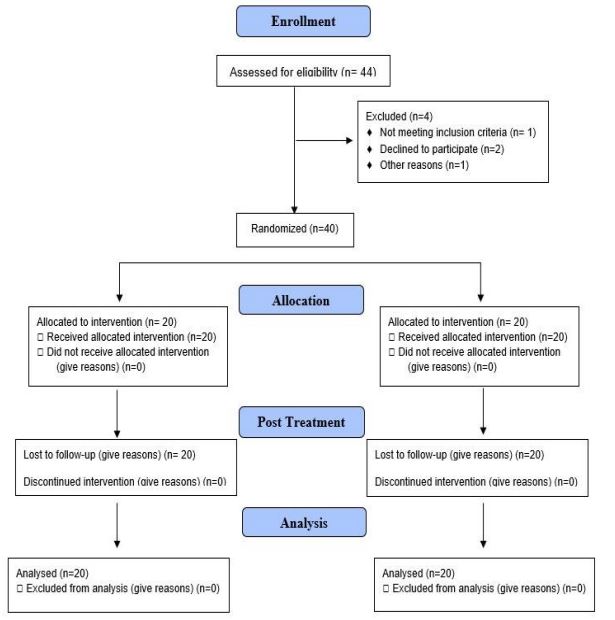
Methodology: This RCT compared Neuromuscular training (NMT) to Closed Chain exercises (CKC) in 40 athletes with acute grade I-II ankle sprains. Participants were randomly assigned to the group that got either CKC exercises (n=20) or neuromuscular training (n=20), 3×/week for 4 weeks. Outcomes measured were pain (Numerical Pain Rating Scale NPRS), range of motion (goniometer), balance (Star Excursion Balance Test), and function (Functional Ankle Ability Measure FAAM), with statistical analyses performed using t-tests (p<0.05). (CTR: NCT06198270
Results: Statistically significant improvement occurred in pain, balance, ROM, and function for 2 groups (p<0.001). Pain reduction was better in the KT group (1.3±0.17 vs. 3.6±0.67), along with superior ROM gains on dorsiflexion (3.7°±1.8° vs. 2.5°±1.4°), on plantarflexion (6.8°±2.4° vs. 3.7°±2.2°), balance (20.6cm±3.7cm vs. 11.7cm±3.0cm SEBT), and function (16.9%±3.4% vs. 5.5%±1.7% FAAM-S) compared with the CKC group (all p<0.001). Hence, neuromuscular training was more effective than CKC exercises for some clinical variables.
Conclusion: Given that both therapies brought great improvements in pain, ROM, balance, and functional outcomes, those patients undergoing neuromuscular training were, in fact, more effective than the other groups, especially in improving balance and functional activities.
Keywords: Athletes, Closed Kinetic Chain Exercise, Functional Disability, Neuromuscular Training
Introduction:
Ankle sprains are one of the most common musculoskeletal injuries in athletes and are caused mainly by inversion during dynamic movement, change of direction, and jump.1 The injuries predominantly affect the lateral ligament complex, with emphasis on the anterior talofibular ligament.2 Confirmed risk factors include prior sprains, neuromuscular deficits, proprioception deficits, muscular weakness, wrong footwear, and uneven playing surfaces, while other contributing factors in this vein are sex, joint laxity, and foot morphology.3
This injury claims for about 15-20% of all sport-related trauma, as ligaments are stretched to the extent of their biomechanical requirements in the field of football.4 Far from being recurrent in the instances of sprains for 70% of the injured athletes, it is mostly due to improper rehabilitation processes or ongoing instability.5 Lateral ankle sprains account for more than 80% of injuries sustained by athletes, with 25-40% recurring within one year, calling forth the glancing attention to bona-fide rehabilitation approaches.5
The clinical assessment of ankle sprains includes a thorough history, consideration of swelling and bruising, and palpation of the Anterior Talofibular Ligament (ATFL), the calcaneofibular ligament (CFL), and distal fibula to identify tenderness.6 Special tests such as the anterior drawer test (to check ATFL integrity) and the talar tilt test (to check CFL involvement) help determine the severity of the injury.7 The Ottawa Ankle Rules indicate whether to proceed with radiographic imaging to exclude fractures. Functional tests such as the Star Excursion Balance Test (SEBT) and single-leg stance help assess proprioception and dynamic stability.8 Pain intensity is scored with the Numeric Pain Rating Scale (NPRS), while functional limitation is measured by the Foot and Ankle Ability Measure (FAAM).9
Acute management follows the POLICE principle to minimize swelling and pain: Protection, Optimal Loading, Ice, Compression, and Elevation. In the subacute stage, rehabilitation involves regaining range of motion (ROM), strength, and neuromuscular control.10 Traditionally, closed kinetic chain exercises (CCE) such as squats and lunges are used to promote joint stability via co-contraction.11 Neuromuscular training (NMT) consisting of proprioceptive exercises, balance perturbations, and sport-specific movements has gained popularity in recent times because it improves dynamic stability and decreases the return-to-injury incidence.12 Options such as Kinesio taping may be applied for augmenting proprioceptive feedback.
NMT is aimed at sensorimotor control with dynamic balance training (e.g., wobble boards, single-leg hops) that enhances proprioceptive acuity and muscle activation timing.13 In comparison, CCE (e.g., leg presses, step-ups) is aimed primarily at strength and endurance with weight-bearing exercises. While CCE improves periarticular muscle strength, NMT addresses impairments in neuromuscular coordination—a primary determinant of recurrent sprains.14 There is increasing evidence that NMT is better at restoring functional performance and decreasing reinjury, yet direct comparison in athletes is limited. The aim of this study is to directly compare their efficacy in pain, joint mobility, balance, and functional recovery.15 Ankle sprains are very common in athletes, with high reinjury rates necessitating the rehabilitation process to be optimized.
This study compares closed-chain exercises (CCE) and neuromuscular training (NMT) for their effectiveness in improving pain, range of motion, balance, and functional return in athletes with acute lateral ankle sprains. Through randomized controlled trial research, we compare the effects of these interventions on clinical and functional measures. The findings provide evidence-based guidance for sports medicine practitioners in managing this common injury. This research bridges a significant gap in sport-specific rehabilitation protocols for athletes.
Methodology:
The randomized controlled trial was carried out at the Pakistan Sports Board, Lahore, from March to August 2023, with the objective of determining the efficacy of two different rehabilitation methods to acute ankle sprain in athletes. The study protocol was duly registered on ClinicalTrials.gov (Identifier: NCT06198270) and was ethically approved by the Research Ethics Committee of Lincoln University Malaysia. All participants gave written informed consent after receiving detailed information regarding the methods employed in the study, risks, and benefits. Confidentiality measures were rigorous to ensure protection of participant data during the study duration.
Thirty players aged 18-30 years were selected on the basis of non-probability convenience sampling. Participants had a minimum of one year of competition experience and a 15-20 hour per week training schedule. Inclusion criteria required a clinical grade I or II lateral ankle sprain diagnosis confirmed through standardized orthopedic tests like Squeeze Test and Talar Tilt Test.16 Exclusion criteria included history of ankle surgery, fracture, or chronic instability with greater than three recurrent sprains. The sample size was calculated using G*Power 3.1 software, with an effect size of 0.65, α error probability of 0.05, and power (1–β) of 0.80, yielding a total sample size of 40 participants.17 Individuals who met the inclusion criteria were randomly assigned to either a control group (n=20) to receive closed kinetic chain exercises or an experimental group (n=20) to receive neuromuscular training.
Outcome Measures: Outcome measures were taken at baseline and following the four-week severity was quantified via the Numeric Rating Scale (0-10), where increased scores reflected increased pain severity.17 Moreover, Ankle range of motion was quantified in terms of standard goniometry for weight-bearing dorsiflexion and non-weight-bearing plantarflexion.18 Dynamic balance was quantified via the Star Excursion Balance Test conducted in three directions: anterior, posteromedial, and posterolateral. Functional performance was assessed through timed 20-meter sprints run on an indoor artificial surface.19
Intervention Protocols: The control group did a progressive closed kinetic chain exercise program that included squats (0-30° knee flexion), multiplanar lunges, bilateral-to-unilateral leg presses at 60-80% of their one-repetition maximum, and step-ups on boxes 10-30 cm. The subjects did these exercises in 3-5 sets of 8-12 repetitions, with 90-second rest intervals between sets. The experimental group received a neuromuscular training program consisting of single-leg standing on various surfaces, dynamic calf raises, heel-to-toe walking patterns, and balance board training designed to enhance proprioceptive awareness and neuromuscular control.
Following each intervention session, participants’ affected ankles were taped with Kinesio tape by licensed physiotherapists using a four-step protocol with 30-40% tension in a sitting position with the feet elevated. The first step was posterior talar gliding taping to facilitate dorsiflexion with the tape being applied from the talus, around both malleoli, to the calcaneus with the ankle in slight dorsiflexion. Phase two was inversion taping, applied 5 cm superior to the medial malleolus and twisting posteriorly and inferiorly around the lateral malleolus prior to crossing the sole laterally to medially in the presence of the ankle in a slight inversion position. The taping for eversion was applied twice with 50% overlap starting 5 cm above the lateral malleolus, going behind and underneath the medial malleolus, and curving medially to laterally under the sole to address restricted inversion caused by lateral ankle sprains. Taping was completed with the posterior talar gliding taping being repeated in order to continue to enhance dorsiflexion.20 All interventions were performed by KT-certified therapists who accomplished skin preparation, uniform tape tension, and proper anatomical alignment, and participants were instructed to leave the tape on between sessions while monitoring skin integrity and tape adhesion.
Statistical Analysis: Statistical analysis was completed with the aid of SPSS version 23, and a significance level of p < 0.05 was considered. The Shapiro-Wilk test ascertained that all outcome measures were normally distributed due to which, parametric statistical tests were applied. Hence, Paired-t test for intra-group and independent-t test for between group comparisons were utilized.
Figure 1: CONSORT Flow Diagram
Results:
The general demographic features of the study participants are explained in Table 1. The study population consisted of 40 sportspersons equally distributed into the Closed Chain Exercise (Group A, n=20) and Neuromuscular Training (Group B, n=20) interventions. The age composition was comparable in both groups, with Group A presenting a mean age of 21.5±3.11 years and Group B presenting a mean age of 22.27±2.58 years. Anthropometric measurements revealed no group difference in weight (Group A: 61.0±9.99 kg; Group B: 62.67±4.42 kg) and height (Group A: 5.57±0.29 feet; Group B: 5.65±0.30 feet).
In terms of gender, the majority of participants were male, with 70% in Group A and 75% in Group B, while females comprised 30% and 25%, respectively. Regarding body mass index (BMI), the majority fell within the normal weight category—85% in Group A and 95% in Group B. A small proportion was underweight, comprising 15% in Group A and 5% in Group B. For leg dominance, the right leg was dominant in most participants, reported by 80% in Group A and 90% in Group B, whereas the left leg was dominant in 20% and 10% of participants, respectively. Concerning the injured leg, right leg injuries were more prevalent in both groups (60% in Group A and 70% in Group B), while left leg injuries accounted for 40% and 30%, respectively.
In Group A, there were significant improvements in all the outcomes that were measured following the intervention. Pain severity, assessed using the Numerical Pain Rating Scale (NPRS), was reduced from a pre-intervention level of 3.9 ± 0.89 to 2.6 ± 0.83 following the intervention, with a mean difference of 1.3 ± 0.03 (p < 0.05). Range of motion (ROM) of the ankle improved significantly; that is, dorsiflexion from 18.7 ± 1.44° to 21.3 ± 1.03° (mean difference 2.5 ± 0.41°, p < 0.05), and plantarflexion from 38.8 ± 1.7° to 42.5 ± 3.2° (mean difference 3.7 ± 2.5°, p < 0.05). Dynamic balance, as indicated by the Star Excursion Balance Test (SEBT), also increased from a mean score of 48.9 ± 7.36 to 60.6 ± 3.9, with a mean difference of 11.7 ± 3.46 (p < 0.05). Also, the functional performance assessment with the Foot and Ankle Ability Measure (FAAM) Sports Subscale indicated an increase from 44.7 ± 4.7 to 50.2 ± 5.07, with the mean difference being statistically significant, 5.47 ± 0.37 (p < 0.05). The results demonstrate that the intervention protocol employed for Group A enhanced pain relief, joint mobility, balance, and functional capacity significantly.
In Group B, the intervention yielded statistically significant results in all the outcomes that were measured. The pain severity, as assessed by the Numerical Pain Rating Scale (NPRS), was significantly decreased from the pre-intervention mean of 4.6 ± 0.97 to 1.0 ± 0.76 following the intervention, with a mean difference of 3.6 ± 0.21 (p < 0.05). Range of motion (ROM) for ankle dorsiflexion improved from 19.9 ± 1.3° to 23.6 ± 1.84°, corresponding to a mean difference of 3.7 ± 0.54° (p < 0.05). Further, the ROM for plantarflexion improved, from 38.1 ± 2.55° to 44.9 ± 2.87°, providing a mean difference of 6.8 ± 0.32° (p < 0.05). Balance, as measured using the Star Excursion Balance Test (SEBT), was also significantly improved from 46.3 ± 6.65 to 66.9 ± 5.4, providing a mean difference of 20.6 ± 1.25 (p < 0.05). The functional performance, as quantified by the Foot and Ankle Ability Measure (FAAM) Sports Subscale, increased from 45.5 ± 6.1 to 62.3 ± 7.5, a statistically significant mean difference of 16.87 ± 1.4 (p < 0.05). The results indicate that treatment in Group B produced notable enhancement in pain reduction, ankle dorsiflexion, dynamic balance, and general functional sports performance.
Between-group analysis demonstrated statistically significant differences in all outcomes measures, suggesting that Group B had higher effects than Group A. Pain severity, assessed by the Numerical Pain Rating Scale (NPRS), demonstrated significantly more improvement in Group B (mean difference: 3.6 ± 0.21) when compared with Group A (mean difference: 1.3 ± 0.03), with a between-groups mean difference of 2.3 ± 0.18 (p < 0.05). As for ankle range of motion (ROM), dorsiflexion increased more in Group B (3.7 ± 0.54°) than in Group A (2.5 ± 0.41°), with a mean difference between groups of 1.2 ± 0.13° (p < 0.05). Likewise, there was a greater increase in plantarflexion in Group B (6.8 ± 0.32°) than in Group A (3.7 ± 2.5°), with a resulting statistically significant mean difference between groups of 3.1 ± 2.18° (p < 0.05). Balance, as measured using the Star Excursion Balance Test (SEBT), exhibited a higher improvement in Group B (20.6 ± 1.25) than in Group A (11.7 ± 3.46), with a between-group difference of 8.9 ± 2.21 (p < 0.05). Functional ability, as measured using the Foot and Ankle Ability Measure (FAAM) Sports Subscale, revealed a significantly greater improvement in Group B (16.87 ± 1.4) than in Group A (5.47 ± 0.37), with a between-group mean difference of 11.4 ± 1.03 (p < 0.05). The results indicate that the treatment provided to Group B was more efficient in decreasing pain and improving ankle mobility, dynamic balance, and functional ability compared to the treatment given to Group A.
| Table 1. Baseline demographic characteristics of study participants in intervention group | ||
| Demographic Characteristics | Closed Chain Exercise (Group A) (n=20) | Neuromuscular Training (Group B) (n=20) |
| Age (years) | 21.5 ± 3.11 | 22.27 ± 2.58 |
| Weight (kg) | 61.0 ± 9.99 | 62.67 ± 4.42 |
| Height (feet) | 5.57 ± 0.29 | 5.65 ± 0.30 |
| Gender, n (%) | ||
| Male | 14 (70%) | 15 (75%) |
| Female | 6 (30%) | 5 (25%) |
| BMI Category, n (%) | ||
| Normal | 17 (85%) | 19 (95%) |
| Underweight | 3 (15%) | 1 (05%) |
| Dominant Leg, n (%) | ||
| Right | 16 (80%) | 18 (90%) |
| Left | 4 (20%) | 2 (10%) |
| Injured Leg, n (%) | ||
| Right | 12 (60%) | 14 (70%) |
| Left | 8 (40%) | 6 (30.6%) |
| Table 2: Group A – Pre and Post Intervention Analysis | ||||
| Tool/Outcomes | Parameters | Mean ± SD | Mean Difference ± SD | p-value |
| NPRS (Pain) | Pre | 3.9 ± 0.89 | 1.3 ± 0.03 | <0.05 |
| Post | 2.6 ± 0.83 | |||
| ROM | Dorsiflexion Pre | 18.7 ± 1.44 | 2.5 ± 0.41 | <0.05 |
| Dorsiflexion Post | 21.3 ± 1.03 | |||
| Plantar-flexion Pre | 38.8 ± 1.7 | 3.7 ± 2.5 | <0.05 | |
| Plantar-flexion Post | 42.5 ± 3.2 | |||
| SEBT (Balance) | Pre | 48.9 ± 7.36 | 11.7 ± 3.46 | <0.05 |
| Post | 60.6 ± 3.9 | |||
| FAAM (Sports Subscale) | Pre | 44.7 ± 4.7 | 5.47 ± 0.37 | <0.05 |
| Post | 50.2 ± 5.07 | |||
NPRS= Numerical Pain Rating Scale, ROM= Range of Motion, SEBT=Star Excursion Balance Test, FAAM= Foot and Ankle Ability Measure, Sports subscale
| Table 3: Group A – Pre and Post Intervention Analysis | ||||
| Tool/Outcomes | Parameters | Mean ± SD | Mean Difference ± SD | p-value |
| NPRS (Pain) | Pre | 4.6 ± 0.97 | 3.6 ± 0.21 | <0.05 |
| Post | 1.0 ± 0.76 | |||
| ROM | Dorsiflexion Pre | 19.9 ± 1.3 | 3.7 ± 0.54 | <0.05 |
| Dorsiflexion Post | 23.6 ± 1.84 | |||
| Plantarflexion Pre | 38.1 ± 2.55 | 6.8 ± 0.32 | <0.05 | |
| Plantarflexion Post | 44.9 ± 2.87 | |||
| SEBT (Balance) | Pre | 46.3 ± 6.65 | 20.6 ± 1.25 | <0.05 |
| Post | 66.9 ± 5.4 | |||
| FAAM (Sports Subscale) | Pre | 45.5 ± 6.1 | 16.87 ± 1.4 | <0.05 |
| Post | 62.3 ± 7.5 | |||
| Table 4: Between-Group Analysis (Group A vs Group B) | ||||
| Tool/Outcomes | Mean Difference (Group A) ± SD | Mean Difference (Group B) ± SD | Between Group Mean Difference ± SD | p-value |
| NPRS (Pain) | 1.3 ± 0.03 | 3.6 ± 0.21 | 2.3 ± 0.18 | <0.05 |
| ROM – Dorsiflexion | 2.5 ± 0.41 | 3.7 ± 0.54 | 1.2 ± 0.13 | <0.05 |
| ROM – Plantarflexion | 3.7 ± 2.5 | 6.8 ± 0.32 | 3.1 ± 2.18 | <0.05 |
| SEBT (Balance) | 11.7 ± 3.46 | 20.6 ± 1.25 | 8.9 ± 2.21 | <0.05 |
| FAAM – Sports Subscale | 5.47 ± 0.37 | 16.87 ± 1.4 | 11.4 ± 1.03 | <0.05 |
Discussion:
This study explored how neuromuscular training and closed kinetic chain exercises impact pain, joint movement, balance, and functional performance in athletes with ankle sprains. After four weeks of training, the group receiving neuromuscular training experienced a more noticeable reduction in pain compared to the other group, suggesting its greater effectiveness for pain relief. Both groups showed improvements in ankle movement, particularly in dorsiflexion and plantarflexion, but the neuromuscular training group achieved more substantial progress in both directions. These findings support the use of targeted exercise programs in managing symptoms of ankle sprain. These results are consistent with studies highlighting the effectiveness of exercise interventions in improving ankle joint mobility.21,22 Another study`s results revealed that the ankle inversion/eversion ROM changes were significantly lower in the Kinesio-taped ankle condition.23
Pain Reduction (NPRS): Group B exhibited a significantly greater reduction in pain scores (mean decrease: 3.6 ± 0.21 points) compared to Group A (1.3 ± 0.03 points; *p* < 0.05). These findings align with previous research, who found that NMT reduced pain more effectively than passive treatments by restoring neuromuscular control.24 Similarly, another study reported that active rehabilitation protocols, including NMT, accelerated pain resolution compared to immobilization or isolated CCE.25 In contrast, a literature observed that CCE alone provided moderate pain relief, while Moreira et al. demonstrated that NMT’s dynamic components (e.g., proprioceptive drills) offered superior analgesic effects by addressing sensorimotor deficits.26 The current results suggest that NMT’s emphasis on neuromuscular re-education may explain its greater pain-alleviating effects compared to traditional CCE.
Joint Mobility (ROM) Improvements (Goniometer) Group B showed significantly greater improvements in dorsiflexion (3.7 ± 0.54° vs. 2.5 ± 0.41°; *p* < 0.05) and plantarflexion (6.8 ± 0.32° vs. 3.7 ± 2.5°; *p* < 0.05) than Group A. These results align with previous research attributing neuromuscular training’s range-of-motion benefits to enhanced proprioception and muscle-tendon flexibility.27 Additional studies have noted that incorporating mobilization techniques improves dorsiflexion more effectively than static interventions alone. Conversely, other research has reported limited range-of-motion gains with isolated conventional exercises, while combining them with dynamic stretching has yielded better outcomes.28 The current study extends these findings, highlighting neuromuscular training’s superiority in restoring functional ankle mobility, likely due to its integrative approach targeting both joint stability and dynamic movement patterns.
Balance Enhancements (SEBT): The NMT group achieved greater dynamic balance improvements (20.6 ± 1.25 units) than the CCE group (11.7 ± 3.46 units; *p* < 0.05). Previous research similarly reported that neuromuscular training’s focus on postural control drills significantly enhances balance in ankle sprain patients.29 Other studies have noted that while conventional exercises improve stability, neuromuscular training’s inclusion of perturbation-based training optimizes proprioceptive feedback.30 This aligns with the present results, suggesting that neuromuscular training’s multifaceted approach—combining strength, coordination, and balance drills—offers distinct advantages over conventional training’s more isolated strengthening focus.
Functional Recovery (FAAM Sports Subscale): Group B demonstrated significantly greater functional improvement (16.87 ± 1.4 points vs. 5.47 ± 0.37 points; *p* < 0.05), highlighting neuromuscular training’s ability to effectively transition patients from rehabilitation to sport-specific demands. Previous research has shown that incorporating functional drills, such as agility tasks, leads to faster return-to-play compared to traditional linear exercises.31 Additional studies have noted that conventional training alone often fails to address multiplanar movement deficits, whereas neuromuscular training better replicates the dynamic demands of athletic performance.32 These findings reinforce neuromuscular training’s effectiveness in restoring sport-specific function and preparing athletes for competition.
Future studies should explore long-term outcomes of neuromuscular training across different athletic populations and injury severities. Clinically, incorporating neuromuscular training into rehabilitation protocols may enhance pain relief, joint mobility, and functional recovery more effectively than conventional methods alone.
Conclusion
NMT outperformed CCE in pain reduction, ROM restoration, balance recovery, and functional rehabilitation in athletes with ankle sprains. These results advocate for NMT’s integration into standard rehabilitation protocols to optimize athletic recovery.
References:
- Memon AG, Chandran SP, Zakir T, Sulaman M. Effects of Neuromuscular Training with and Without Kinesio-Tape on Pain, Range of Motion, Balance and Function in Footballer with Ankle Sprain. Journal of Liaquat University of Medical & Health Sciences. 2025 Mar 27;24(01):38-44.
- Dalmau‐Pastor M, Malagelada F, Guelfi M, Kerkhoffs G, Karlsson J, Calder J, Vega J. The deltoid ligament is constantly formed by four fascicles reaching the navicular, spring ligament complex, calcaneus and talus. Knee Surgery, Sports Traumatology, Arthroscopy. 2024 Dec;32(12):3065-75.
- Meng L, Liang Q, Yuan J, Li S, Ge Y, Yang J, Tsang RC, Wei Q. Vestibular rehabilitation therapy on balance and gait in patients after stroke: a systematic review and meta-analysis. BMC medicine. 2023 Aug 25;21(1):322.
- Elliott J, Heron N, Versteegh T, Gilchrist IA, Webb M, Archbold P, Hart ND, Peek K. Injury reduction programs for reducing the incidence of sport-related head and neck injuries including concussion: a systematic review. Sports medicine. 2021 Nov;51(11):2373-88.
- Ghassi HT, Muntessu DL, Buh FC, Womsi RT, Noumoé DL, Chendjou CB, Forelli F, Douryang M, Tresor GH, Ruslaine TW, Leonel ND. Ankle Sprain Recurrence and Rehabilitation Among Athletes: A Case Study in the West Region of Cameroon. Cureus. 2024 Nov 5;16(11).
- Davulcu CD, Davutluoglu E, Nur AM. Foot and Ankle Trauma. InClinical and Radiological Examination of the Foot and Ankle: The Path to Definitive Diagnosis 2024 Aug 20 (pp. 257-275). Singapore: Springer Nature Singapore.
- Netterström-Wedin F, Matthews M, Bleakley C. Diagnostic accuracy of clinical tests assessing ligamentous injury of the talocrural and subtalar joints: a systematic review with meta-analysis. Sports Health. 2022 May;14(3):336-47.
- Picot B, Fourchet F, Lopes R, Rauline G, Freiha K, D’hooghe P, Valentin E, Hardy A. Low ankle-go score while returning to sport after lateral ankle sprain leads to a 9-fold increased risk of recurrence: a two-year prospective cohort study. Sports Medicine-Open. 2024 Mar 8;10(1):23.
- Saarinen AJ, Uimonen MM, Suominen EN, Sandelin H, Repo JP. Structural and construct validity of the Foot and Ankle Ability Measure (FAAM) with an emphasis on pain and functionality after foot surgery: a multicenter study. The Journal of Foot and Ankle Surgery. 2022 Jul 1;61(4):872-8.
- Bhatnagar S, Seth S. Integrating Rehabilitative and Palliative Care Principles Within Acute Care Practice. InPerioperative Care of the Cancer Patient 2023 Jan 1 (pp. 478-488). Elsevier.
- Forelli F, Mazeas J, Korakakis V, Ramtoola H, Vandebrouck A, Duffiet P, Ratte L, Kakavas G, Bouzekaroui Alaoui I, Douryang M, Bjerregaard A. Criteria-Based Decision Making for Introducing Open Kinetic Chain Exercise after-ACL Reconstruction: A Scoping Review. Sports Medicine-Open. 2025 Apr 12;11(1):37.
- Behm DG, Granacher U, Warneke K, Aragão-Santos JC, Da Silva-Grigoletto ME, Konrad A. Minimalist training: is lower dosage or intensity resistance training effective to improve physical fitness? A narrative review. Sports Medicine. 2024 Feb;54(2):289-302.
- Căsăneanu M, Mihăilescu LN, Potop V, Mihăilă I, Manole C, Mihăilescu LE, Rață BC, Mâță L, Rață M. The Role of Climbing Exercises in Developing Balance Ability in Children. Applied Sciences. 2025 May 26;15(11):5959.
- Nyland J, Pyle B, Richards J, Yoshida K, Brey J, Carter S. A clinical practice review of therapeutic movement-based anterior cruciate ligament reconstruction return to sports bridge program: the biological, biomechanical and behavioral rationale. Annals of Joint. 2023 Jul 3; 8:23.
- Verhagen E. Prevention Strategies of Ankle Injuries. InOrthopaedic Sports Medicine: An Encyclopedic Review of Diagnosis, Prevention, and Management 2024 Apr 16 (pp. 1-15). Cham: Springer International Publishing.
- Beynon A, Le May S, Theroux J. Reliability and validity of physical examination tests for the assessment of ankle instability. Chiropractic & Manual Therapies. 2022 Dec 19;30(1):58.
- Noureen A, Ahmad A, Fatima A, Fatima SN. Effectiveness of mirror therapy on management of phantom limb pain and adjustment to limitation among prosthetic users; A single blinded randomized controlled trial. Journal of Bodywork and Movement Therapies. 2025 Jun 1; 42:236-42.
- Koshino Y, Takabayashi T, Akuzawa H, Mizota T, Numasawa S, Kobayashi T, Kudo S, Hikita Y, Akiyoshi N, Edama M. Differences and relationships between weightbearing and non-weightbearing dorsiflexion range of motion in foot and ankle injuries. Journal of Orthopaedic Surgery and Research. 2024 Feb 3;19(1):115.
- Amiri B, Zemková E. Fatigue and recovery-related changes in postural and core stability in sedentary employees: a study protocol. Frontiers in Physiology. 2024 Dec 24; 15:1490041.
- Halabchi F, Hassabi M. Acute ankle sprain in athletes: Clinical aspects and algorithmic approach. World journal of orthopedics. 2020 Dec 18;11(12):534.
- Vallandingham RA, Gaven SL, Powden CJ. Changes in dorsiflexion and dynamic postural control after mobilizations in individuals with chronic ankle instability: a systematic review and meta-analysis. Journal of athletic training. 2019 Apr 1;54(4):403-17.
- Yin Y, Yu Z, Wang J, Sun J. Effectiveness of the rehabilitation training combined with maitland mobilization for the treatment of chronic ankle instability: A randomized controlled trial. International Journal of Environmental Research and Public Health. 2022 Nov 20;19(22):15328.
- Qin Y, Li M, Han J, Cui G, Du W, Yang K. Research hotspots and trends of Kinesio Taping from 2011 to 2020: a bibliometric analysis. Environmental Science and Pollution Research. 2023 Jan;30(1):2029-41.
- Parker C, Robinson K, Lydon K, Schmidt R, Pierre ES, Springer M, Villm A, Sells P. Investigation of a Three-Week Neuromuscular Training Intervention on Biomechanical Parameters of the Lower Quarter in Female Collegiate Pivoting Athletes. Open Access Library Journal. 2022 Dec 1;9(12):1-23.
- Stephanie Reischl RM. Early Neuromuscular Stimulation and Mirror Therapy Interventions to Prevent Functional Loss During Immobilization of Distal Radius Fractures. (Doctoral dissertation, 2024)
- Treleaven J. Management of Sensorimotor Control in Musculoskeletal Disorders. Grieve’s Modern Musculoskeletal Physiotherapy E-Book: Grieve’s Modern Musculoskeletal Physiotherapy E-Book. 2024 Apr 2:374.
- Kim Y, Kim H, Jung J, Lee S. Synergistic Effects of Joint-Biased Rehabilitation and Combined Transcranial Direct Current Stimulation (tDCS) in Chronic Ankle Instability: A Single-Blind, Three-Armed Randomized Controlled Trial. Brain Sciences. 2025 Apr 27;15(5):458.
- Ahmed F, Hossain KA, Islam MS, Hassan MN, Nahid ZB, Uddin MK, Islam MW, Haque MO. The effects of closed kinetic chain exercise on pain and physical function in patients with knee osteoarthritis: a narrative review. Bulletin of Faculty of Physical Therapy. 2023 Nov 15;28(1):48.
- Forelli F, Le Coroller N, Gaspar M, Memain G, Kakavas G, Miraglia N, Marine P, Maille P, Hewett TE, Rambaud AJ. Ecological and specific evidence-based safe return to play after anterior cruciate ligament reconstruction in soccer players: a new international paradigm. International journal of sports physical therapy. 2023 Apr 2;18(2):526.
- Omofuma I. Effects of Perturbation-Based Balance Training and Transcutaneous Spinal Cord Stimulation on Postural Balance Control in Healthy Subjects. Columbia University; 2022.
- Fontanier V, Vergonjeanne M, Eon P, Bruchard A, Laplaud D. Effect of open kinetic chain exercises during the first weeks of anterior cruciate ligament reconstruction rehabilitation: a systematic review and meta-analysis. Physical Therapy in Sport. 2025 Feb 15.
- Godar T. A Mixed-Methods Investigation of a Comprehensive Clinical Examination in an Accredited Athletic Training Program. Lindenwood University; 2022.
| Copyright/Licensing PolicyAll Articles are made available under a Creative Commons “Attribution-NonCommercial 4.0 International” license. (https://creativecommons.org/licenses/by-nc/4.0/). Copyrights on any open access article published by Journal Riphah college of Rehabilitation Science (JRCRS) are retained by the author(s). Authors retain the rights of free downloading/unlimited e-print of full text and sharing/disseminating the article without any restriction, by any means; provided the article is correctly cited. JRCRS does not allow commercial use of the articles published. All articles published represent the view of the authors and do not reflect the official policy of JRCRS. |